Participation experience in self-care program for type 2 diabetes: A mixed-methods study
Article information
Abstract
Purpose
This study aimed to explore the participation experiences of patients with type 2 diabetes in an Automated Personalized Self-Care program, assess the changes in self-care behavior and glycemic control, and evaluate the stages of change and readiness to change using the transtheoretical model (TTM).
Methods
We examined 16 patients with type 2 diabetes who participated in a diabetes self-care program using a mobile application. Purposive sampling continued until data saturation. Using a mixed method study, we analyzed the participants’ characteristics, self-care behavior, stage of change, and readiness to change quantitatively and analyzed the qualitative data using Elo and Kyngas’s content analysis method.
Results
The compliance group (CG) showed improved self-care behavior and glycemic control. In the CG, the proportion of participants in the action stage was higher in the exercise and diet domains and lower in the blood glucose testing and medication domains than in the non-compliance group (NCG). Readiness to change, motivation for health behaviors, and social motivation were higher in the CG, whereas personal motivation was higher in the NCG. In this qualitative study, three categories and 11 subcategories were identified. The findings suggest the CG regarded their experience in the program more frequently as positive, whereas the NCG perceived greater barriers to using the mobile application in the program.
Conclusion
Based on the differences identified between the CG and NCG, TTM-based strategies are needed to facilitate the progression of NCG to the action stage.
INTRODUCTION
Worldwide, the prevalence of diabetes among individuals aged 20~79 years was estimated to reach 537 million in 2021 and is expected to rise to 783 million by 2045 [1]. In 2020, one in six adults (16.7%) aged 30 years or older were observed to have diabetes [2], representing a 24.3% increase in the number of patients with diabetes over a period of 5 years from 2017 to 2021 [3]. Diabetes is a chronic condition that requires continuous management to prevent complications, such as neuropathy, nephropathy, retinopathy, foot ulcers, and cardiovascular diseases [4]. Diabetes self-care is integral to preventing complications, indicating active participation in maintaining and improving health and well-being [5]. The World Health Organization has emphasized the significance of self-care in diabetes management by incorporating a healthy diet, regular physical activity, and weight management to control the blood glucose (BG) levels [6].
Interventions utilizing mobile applications (apps) have been widely developed to promote diabetes self-care. These interventions involve the tracking of self-care behaviors and providing patients with reminders to take medications or measure their BG levels [5]. Additionally, these interventions offered recommendations based on the patients’ knowledge, health status, and current self-care levels, and enabled patients to set their goals, share diaries with others, and foster empathy and connection [7]. Interventions utilizing mobile apps have demonstrated beneficial effects on self-care behaviors, BG, and hemoglobin A1c (HbA1c) levels in patients with diabetes [5,7]. However, a meta-analysis reported that 43.0% of participants did not fully participate in a mobile app intervention [8], and in a dietary self-monitoring intervention, only 13.6% of participants uploaded photos for monitoring at least once per week [9]. Some participants initially expressed willingness to participate; however, after experiencing a decline in participation, they discontinued the intervention prematurely [10]. Therefore, strategies are needed to improve the participation of patients with diabetes in mobile app interventions to maximize their effectiveness in supporting self-care.
Previous studies have explored factors related to the participation in interventions utilizing apps for patients with type 2 diabetes mellitus (T2DM). Factors, such as health status, support from healthcare providers and relatives, awareness of app usage, and understanding of disease severity, technical literacy, and internet connectivity can influence participation in these interventions [11,12]. However, some studies only included participants with excellent disease management [11] or analyzed participants who had used an app as part of the intervention group [12]. In light of this, there is a lack of research comparing the experiences of individuals with low participation in utilizing apps with those with higher participation. Comparing their experiences can provide insights into understanding patients with low participation in app usage, which is essential for devising effective strategies to enhance their participation.
Several studies have used specific models to assess and evaluate the self-care in patients with diabetes. One of these models is the transtheoretical model (TTM), which states that the readiness to change is a determining factor in participating in and maintaining health-promoting behaviors and that individuals have the potential to progress and regress throughout the stages of readiness to change [13]. Applying the TTM to assess and evaluate participants’ self-care can enhance our understanding of their readiness to change and factors contributing to their low or high participation. Moreover, planning motivational strategies based on the participants’ readiness to change can contribute to progressing to the next level and improving intervention compliance [14]. In a previous study, providing a consistent intervention regardless of the participants’ readiness to change their self-care behavior resulted in a decrease in intervention compliance within 6 months [15].
Participation in the intervention refers to understanding the purpose of the intervention and adhering to the plan, and compliance indicates that the participants adequately fulfilled their involvement in the intervention [10]. In this study, compliance was defined as the extent to which participants performed self-care behaviors and recorded them using an app. Those achieving a compliance rate of 80.0% or higher were categorized into the compliance group (CG), whereas those with a compliance rate below 80.0% were classified into the non-compliance group (NCG). We qualitatively and quantitatively analyzed both groups based on the TTM to assess changes in self-care behavior and glycemic control, explore the participation experience of the self-care program using a mobile app, and identify factors that influence sustained participation. Specifically, we analyzed the participants’ characteristics, changes in self-care behavior and glycemic control, stage of change, and readiness to change quantitatively, and qualitatively explored participants’ positive or negative experiences and barriers related to intervention participation.
METHODS
Ethic statement: This study was approved by the Institutional Review Board (IRB) of Pusan National University Yangsan Hospital (IRB No. 04-2021-052). Informed consent was obtained from the participants.
1. Study Design
This study used a mixed-methods research design to analyze the experiences of patients who participated in an app-based self-care program developed by our research team [16]. As a complementary method to qualitative analysis, a quantitative analysis was conducted to analyze the participants’ characteristics, self-care behaviors, glycemic control, stage of change, and readiness to change, with a focus on confirming the results based on the qualitative findings [16]. Qualitative and quantitative data are expected to provide a comprehensive understanding and insight into contexts and meanings that may be challenging to capture through qualitative or quantitative data alone. This study was described following the consolidated criteria for reporting qualitative research (COREQ) [17].
2. Setting and Samples
The participants were patients with T2DM from Pusan National University Yangsan Hospital who participated in an Automated Personalized Self-Care (APSC) program [18]. The inclusion criteria for the APSC program were: T2DM diagnosis, age of 40~69 years, HbA1c levels ≥7.0% within the last 3 months, use of an Android smartphone, and the ability to walk without assistive devices [18]. The participants in this study had a minimum of 6 months of program participation, as this is generally considered the duration required for behavior change [15]. The participants who understood and agreed with the purpose and methods of the study were selected. In this study, we qualitatively analyzed the participation experience of CG and NCG to explore factors related to sustained participation, and, as a complementary method, conducted a quantitative investigation to support the qualitative research findings [16]. Therefore, the sample size was determined based on the saturation of the qualitative research data, indicating that no new information emerged.
This study included 16 participants who participated in the APSC program from January to August 2022, and none refused to participate in the interviews. Successful program execution was defined as achieving 80.0% or more of the recommended frequency in a previous study [19]. We instructed the participants to record their self-care data on the app for at least 5 days per week. Therefore, the participants who input data 4 days or more per week, which is 80.0% of the recommended frequency of app usage, were classified into the CG, whereas those who input data less than 4 days per week were classified as the NCG. The CG and NCG participants were purposively selected based on their compliance levels over the previous 6 months.
3. Measurement
1) Characteristics of Participants
The participant characteristics were measured in terms of sex, age, marital status, employment status, monthly income, duration since DM diagnosis, DM treatment method, and comorbidities.
2) Self-Care Behaviors and Glycemic Control
The self-care behaviors were measured using diabetes self-care behaviors and physical activity. Diabetes self-care behaviors were measured using the Korean version of the Revised Summary of Diabetes Self-Care Activities (SDSCA) [20]. The scores were calculated as the frequency of self-care activities per week, with higher scores indicating better self-care. Cronbach’s α in this study ranged from .16 to .84. Physical activity was evaluated using the Korean version of the International Physical Activity Questionnaire. There were continuous and categorical scores on the International Physical Activity Questionnaire. A continuous score was obtained by multiplying the metabolic equivalent task score, physical activity frequency, and duration (in minutes) of walking, moderate-intensity activity, and vigorous-intensity activity. Additionally, according to the total volume and number of days of each activity, individuals were categorized as inactive, minimally active (e.g., 5 or more days of moderate-intensity activity or walking for at least 30 minutes per day), or health-enhancing level of physical activity (e.g., vigorous-intensity activity on at least 3 days achieving a minimum of at least 1,500 metabolic equivalent task-minutes per week). The test-retest reliability for each domain ranged from a Spearman’s Rho Coefficient of 0.30~0.61, and validity compared to accelerometer data demonstrated a Pearson’s Correlation Coefficient of 0.43 [21]. The glycemic control was assessed using BG and HbA1c levels from electronic medical records. The pre-test data up to 3 months before data collection were compared with the 6-month follow-up data collected within the subsequent 3 months.
3) Stage of Change and Readiness to Change
The stage of change was assessed using a single question about the participants’ intention to participate in regular diabetes self-care within the next 6 months. Based on the participants’ responses, they were categorized as pre-contemplation, contemplation, preparation, action, or maintenance [13]. ‘Readiness to change’ identifies the motivation to change [22], including motivation for health behavior [23], personal motivation, and social motivation [24]. The motivation for health behavior was measured by assessing the participants’ cognitive evaluation of the effectiveness, benefits, and barriers to participating in self-care behavior as well as their emotional preference for the behavior. Personal motivation was assessed using the third version of the Diabetes Attitude Scale, which consists of nine questions designed to measure the internal factors, such as attitudes and beliefs about health. Cronbach’s α was .63 to .74 in the study of Choi [25] and .58 to .65 in this study. Social motivation was measured using the Diabetes Family Behavior Checklist-2 [7], consisting of five questions designed to measure the positive support for self-care from family and neighbors. Cronbach’s α was .84 in the study of Jeon and Park [7] and .80 in this study.
4. Qualitative Data Collection
To obtain qualitative data, the female principal researcher (MK), a master’s student in nursing, explained the purpose of this study to patients waiting for an outpatient medical consultation who had never met before the interview. The principal researcher conducted face-to-face interviews with participants who agreed to participate. Before starting the interview, the researcher explained who she was, why she was interested in this research question, and adopted an attitude aimed at understanding the participant’s experience. The researcher began by asking participants about their recent health conditions and BG management to help them become comfortable with the conversation and build trusting relationships. The interviews were conducted for 20 to 35 minutes in a quiet outpatient consultation room to ensure confidentiality of the interview content. All processes were recorded using digital recording appliances while the notes were written. The semi-structured interview began with an open-ended question: “How was your experience participating in the diabetes management program using the app for 6 months?” The semi-structured questions were developed based on the previous literature and reviewed by a professor and a doctoral student for validation. During the interviews, additional questions were asked if anything was ambiguous or not understood, and the content of the interviews was summarized. We received feedback from the participants and conducted interviews until data saturation was achieved.
5. Intervention
The APSC program was developed for patients with T2DM to efficiently manage self-care. It closely monitors the participants’ self-care status and utilizes algorithms to provide personalized care, including customized goals and automated feedback. The participants engaged in exercise, followed a specific diet, underwent BG testing, adhered to medication, and were recorded on the app. They received (1) personalized goals, (2) education, (3) monitoring, and (4) feedback through the intervention. The initial exercise goal was set at 50 minutes per day. The dietary goal was determined by calculating the appropriate calories by multiplying the standard body weight with the activity level. The goal of the medication was 100.0% adherence; additionally, BG monitoring was performed at least once a day.
Education was conducted focusing on the necessity and methods for managing diabetes. A monitoring reminder was sent daily at 8 PM. The goal achievement graphs were displayed on the home screen, allowing users to check their status easily. The feedback was sent at 8 AM regarding the highest and lowest goal achievement rates of self-care behaviors on the previous day. In addition, the research team encouraged daily self-care and app-based monitoring through calls or messages, aiding goal setting, checking participants’ learning, and providing positive feedback and complication risks [18].
6. Data Analysis
Quantitative data were analyzed using SPSS, version 26.0 (IBM Corp.). The participants’ characteristics, levels of self-care behavior, glycemic control, stage of change, and readiness to change in the CG and NCG were analyzed in terms of the frequency, percentage, mean, and standard deviation.
Qualitative data were transcribed and analyzed using an inductive content analytic technique following the approach outlined by Elo and Kyngäs [26]. First, all possible meaningful content was identified in the data to be analyzed and organized into a statement, and the selected meaningful content was written on coding cards. Second, the generated coding cards were grouped into common patterns and meanings, and organized into subcategories. Finally, the generated subcategories were integrated based on their meanings and abstracted into high-level categories. The entire research process and analysis results were reviewed by a nursing professor with extensive experience in qualitative research, and the key statements, codes, and categories were repeatedly revised. This study followed the trustworthiness criteria of Lincoln and Guba [27]. The researcher and the nursing professor cross-verified the participants’ statements to ensure credibility. Data collection was stopped in the participant interviews when data saturation was confirmed, signifying that there were no further meaningful data for transferability. The principal researcher acquired a foundation in mixed methods and qualitative research through coursework, and actively participated in seminars and workshops for dependability. The comprehensive application of content analysis was carried out, along with pre- and post-analysis reflections to maintain neutrality for confirmability.
7. Ethical Considerations
This study was approved by the Institutional Review Board (IRB) of Pusan National University Yangsan Hospital (IRB 04-2021-052). The principal researcher informed the participants about the purpose, methods, benefits, and risks of the research; the necessity of audio-recording interviews; privacy and confidentiality assurances; and the right to refuse involvement, according to the Helsinki Declaration. Subsequently, the researcher obtained written informed consent from all participants.
RESULTS
1. Participant Characteristics, Levels of Self-Care Behaviors and Glycemic Control
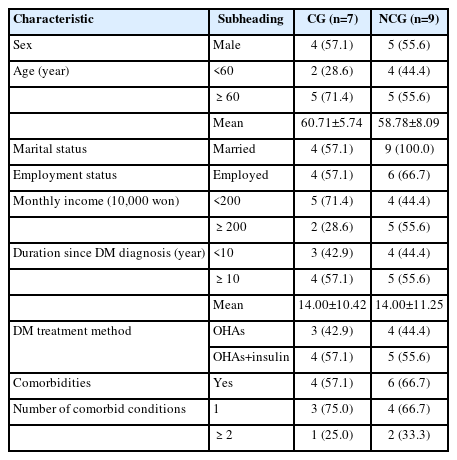
The participant characteristics are summarized in Table 1. In the CG and NCG, male accounted for 57.1% and 55.6%, respectively, and the mean ages were 60.71 and 58.78 years, respectively. All participants in the NCG were married, while only 57.1% in the CG were married. Regarding the monthly income, 71.4% of the CG earned less than two million won, whereas 55.6% of the NCG earned two million won or more. Both groups had a mean diabetes diagnosis duration of 14.00 years. The treatment methods used were oral hypoglycemic agents and insulin combination therapy in 57.1% of the CG and 55.6% of the NCG. The proportions of participants with comorbidities were 57.1% and 66.7% in the CG and NCG, respectively.
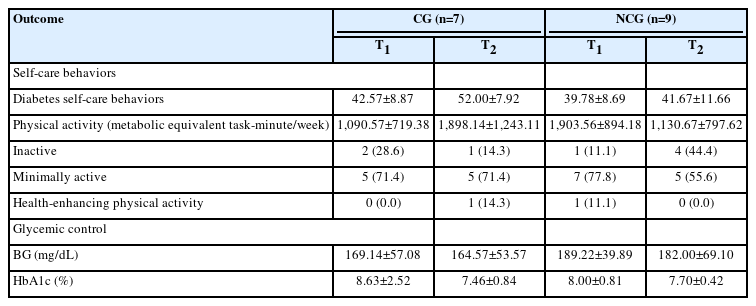
The levels of self-care behaviors and glycemic control of the participants in the CG and NCG are shown in Table 2. In the CG, diabetes self-care behaviors were 42.57 at baseline, increasing to 52.00 after 6 months, while in the NCG, the behaviors increased from 39.78 to 41.67. In the CG, the proportion of minimally active was maintained at 71.4% and health-enhancing level of physical activity increased from 0.0% to 14.3%. In the NCG, the proportion of minimally active decreased from 77.8% to 55.6%, and that of inactive individuals increased from 11.1% to 44.4%.
In terms of glycemic control, BG slightly decreased from 169.14 to 164.57 mg/dL in the CG and from 189.22 to 182.00 mg/dL in the NCG. While the HbA1c level (%) was higher in the CG (8.63) than in the NCG (8.00) at baseline, it was 7.46 in the CG and 7.70 in the NCG after 6 months, with the CG demonstrating a lower level.
2. Health Behavior Monitoring, Stages of Change, and Readiness to Change of the Participants at the 6-Month Follow-Up
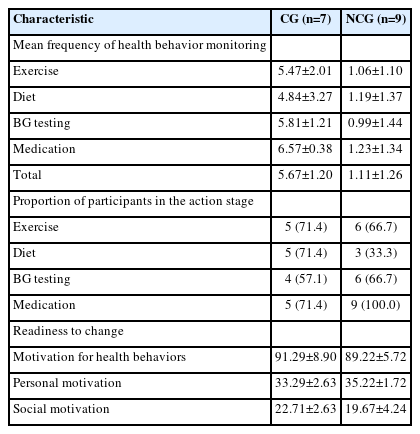
Table 3 presents the health behavior monitoring using the app, the proportion of participants in the action stage for each self-care, and the readiness to change at the 6-month follow-up. Overall, the CG had a higher monitoring frequency (5.67 times per week) than the NCG (1.11 times per week). The CG also had a higher proportion of participants in the exercise and diet action stages. In terms of the readiness to change, the CG showed slightly higher motivation for health behaviors and social motivation, whereas the NCG showed slightly higher personal motivation.
3. Qualitative Results
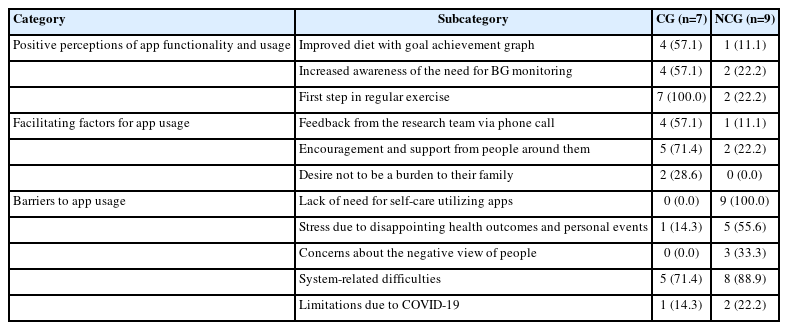
After analyzing the interview data, 185 key statements were categorized into 35 codes, which were grouped into 11 subcategories. Three main categories were derived from the data: positive perceptions of app functionality and usage, facilitating factors for app usage, and barriers to app usage (Table 4). Positive perceptions of the app functionality and usage were more common in the CG than in the NCG. The primary barrier for the NCG was “lack of need for self-care utilizing an app.” Notably, the CG highlighted positive perceptions such as “improved diet,” “increased BG monitoring,” and “first step in regular exercise.” Both groups identified “system-related difficulties” as a major barrier.
1) Positive Perceptions of App Functionality and Usage
Three subcategories reflecting the positive perceptions of app functionality and usage were identified: (1) improved diet with a goal achievement graph, (2) increased awareness of the need for BG monitoring, and (3) the first step in regular exercise. The subcategory (3) was highly prevalent (100.0%) in the CG.
(1) Improved diet with goal achievement graph
The CG (57.1%) and NCG (11.1%) identified and adjusted their food intake to address the deficiencies in specific food groups, while reducing excessive consumption. Additionally, tracking the calorie content when entering meals in the app proved to be beneficial for diabetes management.
“I was uncertain about how to regulate my meals... and unsure if my current food intake was appropriate... However, (after using the app) I realized that I was consuming more than twice the recommended amount.” (Participant 2)
(2) Increased awareness of the need for BG monitoring
The CG (57.1%) and NCG (22.2%) increased their awareness of BG management and made efforts to measure their BG levels regularly, including those who did not do so daily.
“I find myself conducting glucose tests more frequently than before because I need to input (the BG data) in the app... Whenever the app displays high readings, it increases my awareness of the importance of monitoring my BG levels.” (Participant 15)
(3) First step in regular exercise
The CG (100.0%) and NCG (22.2%) recognized the significance of management through app-based exercise target graphs and educational materials, motivating them to incorporate self-care into their daily lives. They gradually implemented these actions in a personalized manner.
“I have started to incorporate more exercise into my routine. Because of my job, it is difficult for me to follow a regular exercise schedule. However, whenever I have some free time during my shifts, I make an effort to walk and climb hills.” (Participant 15)
2) Facilitating Factors for App Usage
The three major facilitating factors for app usage were (1) feedback from the research team via phone calls, (2) encouragement and support from people around them, and (3) desire not to be a burden to their family. The subcategory (2) was prominent in the CG (71.4%).
(1) Feedback from the research team via phone call
This subcategory was observed in the CG (57.1%) and NCG (11.1%). When receiving calls from the research team, the participants became aware of the consequences of neglecting diabetes management, motivating them to improve their app usage. Feedback based on monitoring records was valuable for identifying the missing or inadequate aspects of BG management.
“The researcher’s continuous attention stimulates us, triggers reflection, and motivates improvement. It reminds me to stay attentive even when I tend to forget about diabetes management.” (Participant 11)
(2) Encouragement and support from people around them
The data regarding this feedback were derived from the CG (71.4%) and the NCG (22.2%). Using the app helped their families realize the importance of diabetes self-care. It provided assistance in planning diabetes-friendly meals, encouraging exercise, and creating a shared interest in BG management.
“My wife pays attention to cooking rice with mixed grains and takes care of side dishes accordingly. The app has been very helpful in adjusting our food choices.” (Participant 15)
(3) Desire not to be a burden to their family
This was observed in two participants in the CG (28.6%). The participants were concerned about the potential complications and burdens resulting from insufficient self-care, especially regarding their children’s well-being. These concerns motivated them to set goals for more effective app usage, which led to increased self-care behaviors and continued app use.
“But now, I have many thoughts like, ‘If I want to live healthy and not be a burden to my children, I need to be even more determined and persistent (in managing my condition).’” (Participant 9)
3) Barriers to App Usage
Five subcategories reflecting the barriers to app usage to using the app were extracted: (1) lack of need for self-care utilizing an app, (2) stress due to disappointing health outcomes and personal events, (3) concerns about the negative views of people, (4) system-related difficulties, and (5) limitations due to COVID-19.
(1) Lack of need for self-care utilizing an app
All non-compliance participants answered that they did not feel the need to use the app (100%). Some considered their current diabetes self-care to be sufficient, whereas others experienced discomfort, fatigue, and forgetfulness while using the app, which in turn led to reduced motivation and questioned the app’s necessity.
“If diabetes had come to me at young age like you, it would have been great to have an app for diabetes management. Now that I’m in my mid-60s, everything feels bothersome. I simply take my medication as prescribed. I make an effort to maintain a balanced diet and participate in some physical exercise.” (Participant 1)
(2) Stress due to disappointing health outcomes and personal events
This was observed in one participant (14.3%) in the CG and five participants (55.6%) in the NCG. Despite their efforts in diabetes self-care, the participants mentioned that unsatisfactory BG results caused stress and hindered app usage. In addition, stress and depression from life events led to a lack of self-care, which contributed to poor app utilization.
“It’s difficult to live... Our business went bankrupt. I used to manage my diabetes well in my own way, but it all fell apart due to stress... I struggle with managing my food intake. When I try to resist the urge to eat, I often find myself eating even more the following day.” (Participant 8)
(3) Concerns about the negative view of people
This was observed in only three participants (33.3%) in the NCG. Despite the participants’ initial intention to share their diabetes management efforts using an app with others, they faced negative reactions. This led to self-consciousness about using their phones for diabetes management, subsequently reducing their motivation to use the apps.
“I don’t look at it at all when working, just quickly during lunchtime. I just don’t like sitting and typing information (on my phone). Recording immediately what I ate at the moment is challenging because I feel self-conscious and being noticed by others.” (Participant 16)
(4) System-related difficulties
These data were derived from five participants (71.4%) in the CG and eight participants (88.8%) in the NCG. The main system-related difficulties were a small font size, unfamiliarity with the app, and difficulties in monitoring the dietary intake. Visually impaired participants experienced fatigue owing to the small font size of the app and had difficulty watching educational videos for an extended period. In addition, the participants faced issues with touch functions during data input, requiring multiple touches. First-time app users found it challenging to become accustomed to the complexity and long time required for data input. The participants expressed a desire for a simplified input process when searching for a specific menu item while entering dietary data.
“I still struggle to grasp how to use the app correctly. I think I only understand about 30% of its features.” (Participant 14)
“Like, when I have marinated ribs, I searched for them in the app, but it only showed the option for ‘beef, grilled,’ without a specific category for ribs. This lack of specific options causes confusion for me…” (Participant 13)
(5) Limitations due to COVID-19
This was observed in one participant (14.3%) in the CG and two participants (22.2%) in the NCG. Due to the COVID-19 pandemic, they faced restrictions on physical activities, such as gymnasiums closure and limited outdoor activities, leading to reduced app usage.
“I must admit that I still struggle with it. … I registered for a gym, but lately, due to COVID restrictions, there aren’t many available opening hours for me to go.” (Participant 11)
DISCUSSION
This study aimed to qualitatively and quantitatively explore the participation experiences of patients with T2DM, assess changes in the self-care behaviors and glycemic control, and evaluate the stages of change and readiness to change using TTM. The CG more frequently regarded their experiences with the program as positive, whereas the NCG perceived greater barriers to using the mobile app. The CG showed improved self-care behaviors and glycemic control. The proportion of CG participants in the action stage was higher than that of the NCG participants in the exercise and diet domains. In the readiness to change, motivation for health behaviors and social motivation were higher in the CG. Therefore, TTM-based strategies are required to facilitate the progression of NCG to the action stage.
In our study, the BG and HbA1c levels improved after using the app. Similarly, in a previous study that evaluated the effectiveness of a diabetes self-care app, the postprandial BG levels decreased [7]. An increase in the physical activity levels of the participants in the CG was observed in this study, whereas previous studies did not show an increase in exercise [5,7]. The newly developed APSC program is a valuable strategy for improving physical activity in patients with diabetes. Additionally, social motivation in this study was 22.71 for the CG and 19.67 for the NCG, which were higher than the 13.87 in a previous study [7]. This can be attributed to participants receiving support from their families, as is evident through their engagement in the APSC program.
There was a difference in the physical activity levels between the CG and NCG at the 6-month follow-up. Both groups faced limitations imposed by the COVID-19 pandemic, including lifestyle restrictions and social distancing measures. Nevertheless, the CG employed a counterconditioning strategy to overcome challenging situations, whereas the NCG remained in the cognitive stage, without progressing to the action stage. Similarly, previous research by Hidrus et al. [28] reported the impact of processes of change, such as counter conditioning, on increasing the physical activity by harnessing the positive aspects of individuals’ behavioral changes. Consequently, future investigations should prioritize the exploration of patients’ processes of change within the TTM to identify effective strategies for diabetes management and facilitate and sustain self-care.
In the qualitative analysis of patients’ participation experiences, all participants in the NCG exhibited a “lack of need for self-care utilizing an app.” They demonstrated limited knowledge about the app’s usage and benefits, and often felt discouraged due to a perceived lack of progress, indicating that they were in the pre-action stage. These participants recognized the app’s positive aspects; however, they also expressed concerns about barriers, including inconvenience and discomfort. Conversely, the participants in the CG were mostly in the maintenance stage and reported more positive experiences than barriers to their self-care journey through the app. Therefore, when characteristics associated with the pre-action stage, as described above, are observed, it is essential to provide tailored interventions to facilitate their progression towards the maintenance stage.
In this study, those who considered the app unnecessary expressed the belief that their diabetes was not severe or that their current self-care practices were sufficient. This finding is consistent with that reported by Jeffrey et al. [12]. Additionally, individual beliefs about the app not only affected its usage, but also had implications for HbA1c levels [29]. Therefore, it is imperative to promote the participants’ beliefs about the positive impact of diabetes management apps. Various approaches should be attempted, including promotional campaigns, recommendations by healthcare providers, and facilitating information sharing with professionals via apps.
The main barrier mentioned by both groups was “system-related difficulties.” The first issue was the small font size, which has also been identified as an obstacle in other qualitative studies of app-based self-care for T2DM patients [12,29]. To accommodate participants with visual impairments or older age, it is crucial to modify the app to include larger font sizes. The second challenge was the unfamiliarity and complexity of the app, emphasizing the importance of patient-healthcare professional interactions until the patients became familiar with the app [29]. Minimizing technical issues is essential for preventing the loss of motivation and disengagement in e-health interventions. Therefore, prompt addressing of the participants’ reported technical issues is necessary to ensure their continued use of the app during and after the intervention. Additionally, the participants in this study did not mention any inconvenience regarding internet connections. However, in previous studies, internet connectivity has been mentioned as a barrier to app usage [12]. Therefore, APSC program and internet connectivity are well established.
In the subcategory “encouragement and support from people around them,” social support played a crucial role in facilitating compliance with the app, aligning with the TTM’s emphasis on involving supportive families and friends during the transition from the action to the maintenance stage [14]. In a previous study, family support was associated with an improved treatment compliance in patients [7]. Telephone feedback from the research team was also identified as a facilitating factor for app usage, consistent with prior research indicating that interaction with healthcare professionals increased the app usage among T2DM patients [7,12]. These combined approaches were considered to enhance participant compliance. In addition, participants expressed a desire to communicate with healthcare professionals while using the app [7]; we believe our APSC program is an excellent tool for promoting such behavioral change.
As this study only included a subset of participants from the APSC program, caution is needed when generalizing the findings to all patients with diabetes using self-care apps. However, this study is significant for the identification of the processes and stages of change between the CG and NCG participating in a diabetes self-care program utilizing a mobile app. Tailored intervention for NCG should be considered based on the process and stage of change.
CONCLUSION
Our study revealed that the CG demonstrated higher levels of physical activity, had a positive perception of the app, and employed more behavioral strategies to manage their diabetes. In contrast, the NCG had a higher rate of recognizing the self-care experience of using apps as a barrier than did the CG. All NCG participants perceived a lack of need for self-care utilizing apps because of their limited knowledge of using apps and understanding their benefits, whereas none of the CG participants perceived this. In the stage of change, the CG had a higher action rate in exercise and diet than the NCG.
These findings highlight the importance of tailoring interventions to the NCG by considering the process and stages of change. We also identified the patient characteristics and participation experiences that have the potential to enhance intervention compliance. Based on these results, researchers should prioritize efforts to improve participants’ intervention compliance.
Notes
Authors' contribution
Study conceptualization and methodology - MK and HL; Data collection and analysis - MK and GP; Drafting and critical revision of the manuscript - MK, HL, GP, and ARK; Supervision - HL and ARK; All authors have read and agreed to the published version of the manuscript.
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This study was a Basic Research Project supported by the National Research Foundation of Korea with funding from the government (Ministry of Education) in 2019 (assignment number: NRF-2019R111A3A01062513).
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
We would like to thank the endocrinology medical staffs at Pusan National University Yangsan Hospital who graciously worked with us and all the participants who participated in this research.