The influence of professional competency, professional commitment, and nursing organizational culture on the person-centered practice of nurses in long-term care hospitals: A cross-sectional study
Article information
Abstract
Purpose
This study aimed to examine the influence of professional competency, professional commitment, and nursing organizational culture on the person-centered practice of nurses in long-term care hospitals.
Methods
A total of 131 nurses in seven long-term care hospitals in Daegu city and Kyeongsang province participated in the study. Professional competency, professional commitment, nursing organizational culture, and person-centered practice were measured using the Nurse Professional Competence Short-Form, Professional Commitment Questionnaire, Nursing Organizational Culture scale, and Korean Measure of Person-Directed Care. Hierarchical multiple regression analysis was used to analyze the data.
Results
Nurses in long-term care hospitals had mean scores of 4.77±0.84 for professional competency and 4.27±0.89 for professional commitment out of a 1~7 scale and 3.45±0.44 for person-centered practice out of a 1~5 scale. Regarding nursing organizational culture, nurses had the highest score in relation-oriented organizational culture and the lowest score in task-oriented culture. Nurses’ professional competency (β=.59, p<.001) and innovation-oriented culture (β=.36, p<.001) were the factors influencing person-centered practice, which explained the variance of 52.5%.
Conclusion
To improve person-centered practice in long-term care hospitals, it is necessary to implement strategies for improving nurses’ professional competency and innovation-oriented nursing organizational culture.
INTRODUCTION
1. The Need for the Research
As the establishment of long-term care hospitals became active in Korea with an increase in the older adult population, the number of long-term care hospitals increased more than 13 times from 113 in 2004 to 1,461 in 2022 [1]. However, there has been growing public interest in the person-centered care practice in long-term care hospitals as questions have been raised about the treatment of patients and the quality of care despite this quantitative expansion in long-term care hospitals. The person-centered care practice refers to perceptions and practices of respecting the values and abilities of the care recipients and providing care to protect human autonomy, independence, and self-esteem, with individualized care as the fundamental principle [2]. Globally, it has been reported that the person-centered care practice reduces nurses' stress and burnout, increases job satisfaction and quality of care [3-5], improves participants' physical function and activities of daily living [6], and reduces depression and helplessness [5]. In Korea, the person-centered care practice was also found to positively affect improving the quality of care in long-term care hospitals [7].
McCormack [8] presented the conceptual framework for older adults to promote the person-centered care practice. Based on this, McCormack and McCance [9] expanded the conceptual framework for the person-centered care practice targeting various medical care providers. According to the conceptual framework of McCance and McCormack [10], the quality of care providers should be considered as a prerequisite to providing the person-centered care practice, and expected results can be reached effectively through the person-centered care practice process when a care environment for delivering the person-centered care practice is established. Care providers' qualities include professional competence, which refers to the knowledge, skills, and attitudes of health care providers who provide holistic care, interpersonal skills, beliefs, and values, as well as professional commitment to patients and families [10]. In addition, for these qualities to be fully realized, nurses must be able to deliver the person-centered care practice through the care environment, which is the context and culture of providing care. This care environment includes systems that support shared decision-making, shared authority, effective employee relations, a supportive organizational structure, the possibility of innovation and risk-taking, and the physical environment [9,10].
Previous research has reported factors that influence the person-centered care practice, such as care competence [11], self-leadership [12], and empowerment [13]. These factors are similar to professional competence and interpersonal skills among the qualities of care providers as identified by McCormack and McCance [9] in their framework for the person-centered care practice, and care competence can be said to be an encompassing concept. Care competence improves the efficiency and quality of medical care [14] and can therefore be essential in implementing the person-centered care practice in long-term care hospitals. In addition, since nurses at long-term care hospitals need professional duties and responsibilities for providing care for older adults [15], professional commitment as nurses is particularly required. In addition, previous research has reported that nurses' work environment [16] and innovation-oriented care organizations' culture [17] influenced the person-centered care practice. Care organizations’ culture refers to the behavioral patterns, norms, and expectations that affect the thinking and behavior of care organizations' members [18], which may motivate the person-centered care practice and a care environment that promotes the process [10].
In this regard, care competence, job commitment, and care organizations' culture, presented in the conceptual framework of McCormack and McCance [9], are presumed to be critical factors of the person-centered care practice in long-term care hospitals. Still, empirical research on them is hard to find. Until now, research on the person-centered care practice in Korea has mainly focused on nurses in general hospitals [17]. Some research on nurses in long-term care hospitals has been conducted piecemeal, such as a survey on nurses' perceptions of person-centered care [19] and a correlation analysis [7] of person-centered care and quality of care services.
Therefore, to promote the person-centered care practice in long-term care hospitals, it is necessary to comprehensively identify the factors affecting the person-centered care practice based on the conceptual framework and seek practical measures. As such, based on McCormack and McCance [9], this research aims to understand the impact of care competence, professional commitment, and care organizations' culture in long-term care hospital nurses on the person-centered care practice. The study findings will be important primary data for establishing a direction to promote the person-centered care practice in the future.
2. Research Purpose
The specific purpose of this research is as follows.
1. To identify long-term care hospital nurses’ care competence, professional commitment, and care organizations’ culture and level of the person-centered care practice;
2. To identify differences in the person-centered care practice according to the general characteristics of long-term care hospital nurses;
3. To examine the correlation between long-term care hospital nurses’ care competence, vocational commitment, care organizations’ culture, and the person-centered care practice; and
4. To examine the impact of long-term care hospital nurses’ care competence, vocational commitment, and care organizations’ culture on the person-centered care practice.
METHODS
Ethics statement: This study was approved by the Institutional Review Board of Kyungpook National University (KNU-2021-0004). Informed consent was obtained from the participants.
1. Research Design
This research is a descriptive correlation study to identify care competence, job commitment, care organizations’ culture, and the person-centered care practice level targeting long-term care hospital nurses and to survey the effects of long-term care hospital nurses' care competence, job commitment, and care organizations' culture on the person-centered care practice.
2. Participants
For data collection for this research, among the long-term care hospitals with more than 200 beds in Daegu City and Kyeongsang Province, three specialized hospitals for older adults operated by cities and provinces and four long-term care hospitals operated by private owners were randomly selected. Long-term care hospitals with more than 200 beds were selected as data collection sites because the Patient Safety Act and the Healthcare Act require hospitals with more than 200 beds to have dedicated personnel for patient safety and medical quality improvement. Nurses working in long-term care hospitals who understood the purpose of the research and agreed to participate in the survey were selected as a convenient sample.
Participants were nurses who provided care to patients in the seven long-term care hospitals; however, those on leave were excluded. Based on previous research that indicated new nurses experience difficulty performing nursing for their first year after graduation [20], this research targeted nurses working at long-term care hospitals for more than 12 months. With a significance level of .05, a median effect size of .15, a test power of .90, and nine control variables and six predictors in hierarchical multiple regression test using the G*Power program (University of Dusseldorf), the sample size required a minimum of 124 people. In this research, data were collected from 133 people considering dropout, and a total of 131 people were included as the final sample, excluding two questionnaires with insufficient responses.
3. Ethical Considerations
This research was approved by the Institutional Review Board of Kyungpook National University (KNU-2021-0004). For the ethical consideration of this research, the researcher obtained consent by emailing or verbally explaining to the participants who contacted the researcher after reading the recruitment announcement and provided a copy of the written consent form to participants while complying with the hospital infection rules due to COVID-19. During the consent process, the researcher explained that the data collected would be kept confidential and used only for research purposes. Participants could discontinue participation at any time during the research if they did not want to continue without penalty.
4. Measures
1) Care Competence
Care competence was measured by translating the Nurse Professional Competence Scale-Short Form (NPC Scale-SF) of Nilsson et al. [21] into Korean. In this research, translation and reverse translation were conducted in Korean through a professional translation agency. The NPC Scale-SF is a tool with a total of 35 questions composed of six subdomains: care, value-based care, medical and technical care, care pedagogics, documentation and administration of care, and development, leadership, and organization of care. Examples of question topics by subdomains include "meeting the basic physical needs of patients,” "showing respect for patient autonomy, integration, and dignity,” "administering drugs independently,” "making sure that information is provided for patients to understand,” "using relevant data in patient records,” and "supervising and educating employees.” The NPC Scale-SF was developed by abbreviating the 88 items of the NPC Scale based on the competence required for nurses presented by the World Health Organization, and content validity and composition validity were secured through confirmatory factor analysis in previous research [21]. Cronbach's α was .70 or more in previous research [21] and .98 in this research.
2) Job Commitment
Job commitment was measured by translating the Professional Commitment Questionnaire (PCQ) by Lachman and Aranya [22], which was developed for hospital nurses, into Korean. This research checked the tool's validity through translation and back-translation into Korean through a professional translation agency. The PCQ consisted of four statements, each scored from 1 ('Not true at all') to 7 (' Very true'). Statements included "I am very loyal to the nursing profession," "Nursing is the best profession for me," "I am proud to tell others about my profession," and "I am very interested in the future of the nursing profession." Each statement was summed and divided by the number of statements to create a total score on a scale of 1~7. The total score ranges from 1 (lowest) to 7 (highest), with higher scores indicating higher job commitment. While developing the original tool, content validity was confirmed by targeting hospital nurses. In previous research, job commitment was found to positively affect the quality of care in terms of sensitivity and empathy for patients. Cronbach's α was .90 in previous research [23], while in this research, it was .92.
3) Care Organizations’ Culture
Care organizations' culture was measured with the care organizations' culture tool developed by Han et al. [18], targeting nurses in general hospitals. The tool was developed to measure nurses’ perceptions of the hospital's organizational culture [18]. It consists of 20 questions in four factors. It consists of five questions to measure relationship-oriented culture, six questions to measure innovation-oriented culture, five questions to measure hierarchy-oriented culture, and four questions to measure task-oriented culture. Each question is answered on a Likert scale ranging from 1 ('Not true at all') to 5 ('Very true'). The scores of the questions for each subdomain were summed up and divided by the number of questions to convert the total score for each subdomain to a 1~5 scale. The higher the score for each type of culture, the stronger the nurses perceived the culture within the organization. In the tool development process, the composition validity was verified through question analysis and factor analysis [18]. The reliability of Cronbach's α by subdomains was relationship-oriented culture .88 and .90, innovation-oriented culture .83 and .85, hierarchical culture .78 and .73, and work-oriented culture .72 and .67, in previous research [18] and in this research, respectively.
4) Person-centered Care Practice
The person-centered care practice was measured with the Korean Measure of Person-Directed Care (K-PDC) tool, which was adapted by Choi and Lee [24] from the Measure of Person-Directed Care developed by White et al. [25] for care providers of hospitalized older adults in healthcare facilities. The K-PDC is a 30-question tool consisting of seven subdomains: autonomy, individuality, understanding of people, supportive relationships, comfort care, working with older adults, and operational management. Each question is answered on a Likert scale ranging from 1 ('Not true at all') to 5 ('Very true'). The scores of the questions for each subdomain were summed up and divided by the number of questions. The total score was converted to a scale of 1 to 5, with a higher total score indicating a higher level of person-centered care practice. The construct validity was confirmed by confirmatory factor analysis in previous research [24]. Cronbach's α was .90 in previous research [26] and .92 in this research.
5) Data Collection
Data were collected from February 11, 2021, to June 7, 2021. After obtaining consent for the purpose and contents of the research from each nursing department's head, the researcher proceeded with the research after first checking whether it was ok to visit their hospitals and obtaining consent. Regarding the research participant recruitment announcement, to prevent group gatherings due to COVID-19, maintain a safe distance, and prevent personal information leakage, each nursing department's head directly announced the research participant recruitment and research purpose and contents in the nursing department's group KakaoTalk room.
After initially explaining and obtaining verbal consent by e-mail or phone from the research participants who contacted the researcher after reading the recruitment announcement, the researcher met ward nurses to explain the purpose, contents, and methods of the research and distributed the questionnaire to the participants who agreed to participate in the research after obtaining their written consent. After informing them that the questionnaire would take about 30 minutes to complete and explaining that there were no particular side effects other than filling out the questionnaire, the nurses were asked to fill out the questionnaire individually while securing the infection rules of each hospital due to COVID-19 and maintaining a safe distance. The researcher collected the completed questionnaires.
6) Data Analysis
Regarding the general characteristics of the participants, frequency, percentage, average, and standard deviation were calculated. The person-centered care practice, care competence, job commitment, and care organizations' culture were presented with average, standard deviation, minimum, and maximum values. Differences in the person-centered care practice according to general characteristics were tested with an independent t-test, one-way ANOVA, and Scheffe's test. Pearson correlation analysis was performed to analyze the relationship between person-centered care practice, competence, job commitment, and care organizations' culture.
Hierarchical multiple linear regression analysis was conducted to examine the effects of care competence, job commitment, and care organizations' culture on person-centered care practice. In the first step of the hierarchical analysis, the age, salary satisfaction , and position of the participants which showed statistical significance on person-centered care practice in the bivariate analysis were entered as dummy variables. Next, the effects of care competence and job commitment on person-centered care practice were analyzed while controlling for general characteristics by introducing variables such as care competence and job commitment in the hierarchical analysis 2-step model. Finally, the effects of care organizations' culture by subdomains on person-centered care practice were analyzed under the control of general characteristics, care competence, and job commitment by additionally introducing the care organizations’ culture for each subdomain in the hierarchical analysis 3-step model. It was confirmed that the model's Durbin-Watson statistic was 1.55, close to 2, and the error term was not autocorrelated. In the scatterplot of standardized residuals, the residuals were randomly scattered based on the mean of .1 and showed homoscedasticity. Regarding the multicollinearity, the tolerance limit was .1 or more, and the variance expansion index was less than 10. The data analysis used the IBM SPSS 26.0 statistical program (IBM Corp.).
RESULTS
1. General Characteristics of the Participants
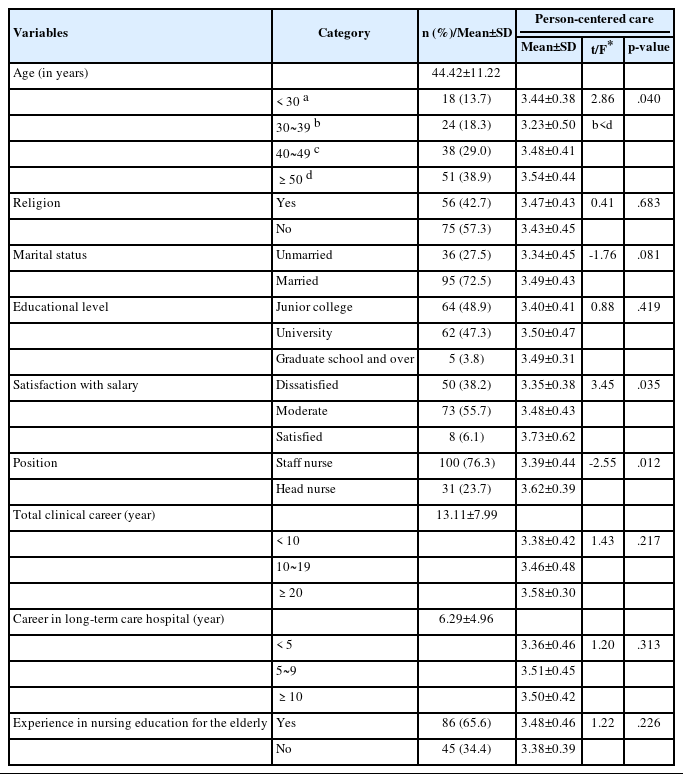
Table 1 shows the general characteristics of the participants. The average age of the participants was 44.42±11.22 years, with 51 (38.9%) being in their 50s or older, followed by 38 (29.0%) being in their 40s, 24 (18.3%) being in their 30s, and 18 (13.7%) being in their 20s. Fifty-six participants (42.7%) were religious, and 95 (72.5%) were married.In the educational level, 64 (48.9%) had a Junior college, 62 (47.3%) had university, and five (3.8%) had a Graduate school and over. As for the participant's salary satisfaction, 73 (55.7%) indicated moderate, 50 (38.2%) were dissatisfied, and eight (6.1%) were satisfied. As for current positions, Staff nurses accounted for 100 (76.3%), and head nurses accounted for 31 (23.7%). The average clinical career of the participants was 13.11±7.99 years, and the average working experience in long-term care hospitals was 6.29±4.96 years. Eighty-six participants (65.6%) had experience in nursing for older adults (Table 1).
2. Participant’s Care Competence, Job Commitment, Care Organizations’ Culture, and Person-centered Care Practice
Table 2 shows the participant's care competence, professional commitment, care organizations' culture, and person-centered care practice level. The participant's care competence was an average of 4.77±0.84 on a scale of 1 to 7. Of subdomains, documentation and administration of nursing care scored the highest at 4.88±0.98, followed by medical and technological care at 4.81±0.85, value-based nursing care at 4.78±0.97, nursing care at 4.72±0.81, Development, leadership, and organization of nursing care at 4.68±1.03, and care pedagogics at 4.67±0.91. The participant's professional commitment averaged 4.27±0.89 on a scale of 1 to 7. The average score of the subdomains of the participant's nursing organizational culture was the highest for the relationship-oriented culture at 3.69±0.65, followed by the hierarchical-oriented culture at 3.37±0.55, innovation-oriented culture at 3.29±0.60, and work-oriented culture at 3.00±0.59. Finally, the participant's person-centered care practice level averaged 3.45±0.44 on a scale of 1 to 5. By subdomain, comfort care scored the highest at 3.87±0.53, followed by knowing the person at 3.62±0.49, working with older adults at 3.54±0.57, personality at 3.52±0.59, management structure at 3.45±0.56, support relationships at 3.22±0.66, and autonomy at 2.89±0.74 (Table 2).
3. Person-centered Care Practice According to the General Characteristics of the Participant
Person-centered care practice showed statistically significant differences according to age (F=2.86, p=.040), satisfaction with salary (F=3.45, p=.035), and job position (t=-2.55, p=.012). The person-centered care practice was higher in participants in their 50s or above than in those in their 30s, in head nurses (vs. staff nurses), and when they were satisfied with their salary. The person-centered care practice of the participants did not differ according to religion, marital status, educational level, hospital clinical career, long-term care hospital clinical career, or elder nursing education experience (Table 1).
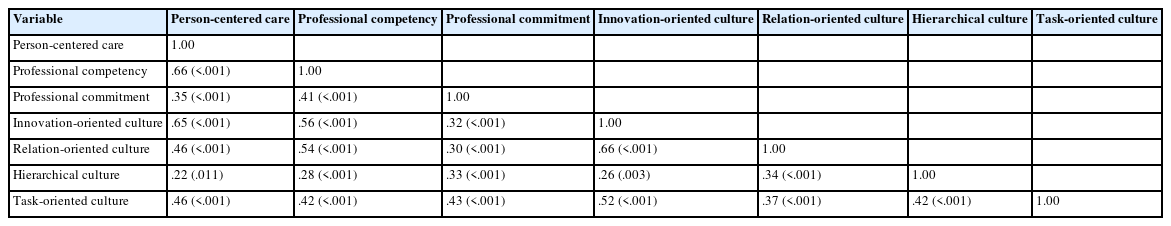
4. Correlation Between Participant’s Care Competence, Job Commitment, Care Organizations’ Culture, and Person-centered Care Practice
Table 3 shows the analysis result of the correlation among the participants’ professional competence, professional commitment, nursing organizational culture, and person-centered care practice. Participants' person-centered care practice was significantly positively correlated with professional competence (r=.66, p<.001) and professional commitment (r=.35, p<.001). Person-centered care practice was positively correlated with innovation-oriented culture (r=.65, p<.001), relationship-oriented culture (r=0.46, p<..001), and task-oriented culture (r=.46, p<.001) among nursing organizational culture, but was not correlated with hierarchical culture (r=.22, p=.011). Participants' professional competence was significantly positively correlated with innovation-oriented culture (r=.56, p<.001), relationship-oriented culture (r=.54, p<.001), task-oriented culture (r=.42, p<.001), and hierarchical culture (r=.28, p<.001) among the nursing organizational culture. Participants' professional commitment was significantly positively correlated with work-oriented culture (r=.43, p<.001), hierarchical culture (r=.33, p<.001), innovation-oriented culture (r=.32, p<.001), and relationship-oriented culture (r=.30, p<.001) among the nursing organizational culture. Also, professional competence and professional commitment were positively correlated (r=.41, p<.001) (Table 3).
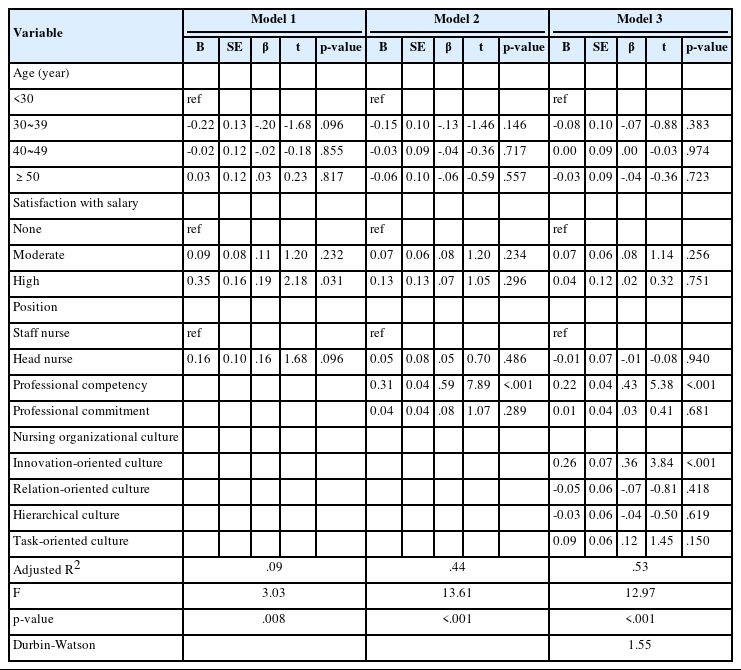
5. Effects of Participant’s Care Competence, Job Commitment, and Care Organizations’ Culture on Person-centered Care Practice
Table 4 shows the results of the hierarchical analysis to identify the effects of the participants’ professional competence, professional commitment, and nursing organizational culture on person-centered care practice. In the hierarchical analysis 1-step model, satisfaction with salary was a significant influencing factor (β=.19, p=.031) on person-centered care practice, and the explanation power was 8.6% (F=3.03, p=.008). In the hierarchical analysis 2-step model, including professional competence and professional commitment and controlling age, salary satisfaction and job position, professional competence was a significant influencing factor (β=.59, p<.001) on person-centered care practice. As a result, the explanation power of the model increased to 43.7% (F=13.61, p<.001). In the hierarchical analysis 3-step model, including nursing organizational culture for each subdomain and controlling age, salary satisfaction, job position, professional competence, and professional commitment, the innovation-oriented organizational culture was a significant influencing factor (β=.36, p<.001) on person-centered care practice. The explanation power of the model was 52.5%, and the additional R2 was 9.7% (F=12.97, p<.001). Care competence, which was significant in the model 2, was still a significant influencing factor (F=5.38, p<.001) on person-centered care practice. In other words, the higher the professional competence and the stronger the perception of the innovation-oriented culture within the nursing organizational, the more positively person-centered care practice was found (Table 4).
DISCUSSION
This research aimed to assess care competence, job commitment, care organizations' culture, and the person-centered care practice of nurses in long-term care hospitals and examine the impact of care competence, job commitment, and care organizations' culture on the person-centered care practice. In this research, nurses' person-centered care practice level in long-term care hospitals averaged 3.45 on a scale of 1 to 5. This was similar to the mean of 3.44 for person-centered care practice measured among nurses in long-term care hospitals in a previous study [18] but lower than the mean of 4.02 for nurses and care aides in older adults’ healthcare facilities [26]. This difference may be attributable to the expansion of human rights education for workers in healthcare institutions according to the 2018 revision of the Enforcement Decree of the Long-Term Care Insurance Act in the case of healthcare facilities and strengthened standards, such as the cancellation of the designation of nursing institutions in the event of abuse [27]. This result suggests that since long-term care hospitals are primarily for patients receiving long-term care, it is necessary to raise nurses' awareness of the person-centered care practice and explore practical measures to move away from medical treatment-oriented care.
Among the subdomains of the person-centered care practice, the autonomy domain scored the lowest, with an average score of 2.89, similar to the average score of 2.90 for long-term care hospital nurses in a previous study [15]. It was also consistent with the lowest autonomy score in healthcare facility nurses in another study [28]. This result means that long-term care hospital nurses do not guarantee free decision-making rights to older adults because they provide uniform and mechanical care [13]. Therefore, it is necessary to prepare measures to support older adults in long-term care hospitals to participate in treatment and care with autonomous decision-making rights.
In contrast, the care competence of long-term care hospital nurses in this research averaged 4.77 on a scale of 1 to 7. Although it is difficult to make a direct comparison due to the lack of previous studies using the same tool, this was similar to the average score of 3.47 for long-term care hospital nurses measured by the 'Ward Nurses Clinical Rating Care Competence Evaluation Tool' on a scale of 1 to 5 [12]. This result suggests that the care competence of long-term care hospital nurses is still at a low level, suggesting that education should be strengthened to improve the competence of long-term care hospital nurses. In addition, the subdomains of care competence, documentation, and management were the highest, with an average score of 4.88, and care pedagogics was the lowest, with an average score of 4.67. Although there is no significant difference between the subdomains, this result suggests that long-term care hospital nurses spend much of their time completing patient assessment sheets, which suggests the need to strengthen patient and family education in long-term care hospitals.
In this research, the average job commitment score of long-term care hospital nurses was 4.27 out of 7, higher than the average of 3.47 for general hospital nurses [28]. Job commitment is high among long-term care hospital nurses because they know their ethical responsibility and duty to care for the patient’s families, as the main participant is older adults [18]. Furthermore, it has been reported that nurses with high job commitment prioritize the health of care recipients and that job commitment increases job satisfaction and lowers the intention to leave [22], which necessitates preparing a plan to enhance job commitment and the occupational identity of long-term care hospital nurses. Although little is known about how nurses' job commitment can be increased, examples of other occupations suggest incentives by motivating them to obtain an advanced certificate or encouraging them to act as members of various professional nursing science and councils [22].
In addition, in this research, the relationship-oriented culture scored the highest at 3.69, and the work-oriented culture scored the lowest at 3.01 on a scale of 1 to 5 in long-term care hospitals culture. This result was similar to that of long-term care hospital nurses in previous research, where the relationship-oriented culture was the highest at 3.48, and the work-oriented culture was the lowest at 3.00 [29]. On the other hand, for the senior general hospital nurses, the work-oriented culture was high at 3.06, and the hierarchical culture was low at 2.46 [30], which was different from the result of this research. This seems to suggest that a work-oriented organizational culture emphasizing the achievement and productivity of organizational goals is emphasized in the care organizations of higher general hospitals, while a relationship-oriented organizational culture centered on flexibility and human relations within the organization prevails in long-term care hospitals. This may mean that vertical and horizontal communication within the care organizations of long-term care hospital nurses is good [23].
In this research, care competence and innovation-oriented care organizations' culture influenced the person-centered care practice significantly. This supports McCormack and McCance's [9] conceptual framework of the person-centered care practice, which identifies care provider quality as an essential antecedent of the person-centered care practice and the importance of the care environment. In addition, this result was similar to previous research in which the care competence of nurses caring for chronically ill patients significantly influenced the person-centered care practice [17]. Therefore, it is essential to have care competence, including care competence and interpersonal skills, to promote the person-centered care practice among long-term care hospital nurses. This suggests that continuous education on the person-centered care practice and systematic support to encourage competent care are necessary.
In addition, the results of this research were consistent with the results of Lee et al.’s study [17] in which innovation-oriented organizational culture was a significant variable for patient-centered care among nurses at local medical centers. Since innovation-oriented organizational culture refers to a culture that recognizes the rapidly changing care environment and emphasizes an attitude that allows new attempts for patient care and can cope with trial and error [23], it is necessary to form an innovation-oriented organizational culture outside the existing framework. Furthermore, transformational leadership has been shown to affect innovation-oriented organizational culture significantly, so care managers must demonstrate leadership in the person-centered care practice to motivate nurses and support them to maximize their potential care competence [23]. On the other hand, in this research, job commitment was significantly related to the person-centered care practice in the correlation analysis but not in the hierarchical analysis. The reason is presumed to be that the job commitment tool mainly measures loyalty and personal satisfaction to the care position and does not measure the degree of commitment to the care work within the organization. Additional research will be needed concerning nurses' job commitment in the future.
The limitations of this research are as follows. Long-term care hospital nurses were self-assessed on care competence, professional commitment, care organizations' culture, and person-centered care practice with a self-report questionnaire, so measurement errors due to subjective reports cannot be ruled out. In addition, since data were collected by convenience sampling from seven long-term care hospitals in Daegu city and Kyeongsang province, care must be taken in interpreting the research results. In addition, due to the cross-sectional data collection, the causal relationship between the variables cannot be confirmed. Nevertheless, this research is meaningful in suggesting an intervention point for future person-centered care practice by confirming the influence of care competence and care organizations' culture on person-centered care practice based on an integrated framework for person-centered care practice. To promote person-centered care based on these results, it is necessary to strengthen long-term care hospital nurses' ability to practice care through continuous education, learning, and information provision and to create an innovation-oriented care organization’s culture that can accept and adapt to changes.
CONCLUSION
After analyzing the influencing factors on the person-centered care practice of long-term care hospital nurses in this research, it was found that long-term care hospital nurses' care competence and innovation-oriented care organizations' culture significantly affected person-centered care practice. Therefore, to promote the person-centered care practice in long-term care hospitals, it is important to take multifaceted measures to promote nurses' care competence and create an organization’s innovative care culture. In particular, it is necessary to provide continuous education on the person-centered care practice and systematic support to promote care competence, including care competence and interpersonal skills. In addition, it is necessary to create an organizational culture that encourages new attempts in the changing care environment and motivates the person-centered care practice. Based on the results of this research, we would like to suggest the following. First, it is necessary to develop a care competence-strengthening program to promote the person-centered care practice of long-term care hospital nurses and verify its effectiveness. In particular, it is necessary to develop person-centered care practice competency enhancement programs such as continuous education and support system development and demonstrate their effectiveness. Second, it is necessary to develop specific strategies to create an innovation-oriented organizational culture in long-term care hospitals, including developing transformational leadership and organizational systems to motivate employees. Third, further research on the causal relationship between the variables is needed by expanding the sample to a national level and collecting longitudinal data.
Notes
Authors' contribution
Study conception and design acquisition - SHK and YSC; Data collection - YSC; Analysis and interpretation of the data - SHK and YSC; Drafting and critical revision of the manuscript - SHK and YSC
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
This article is a revision of the first author's master's thesis from Kyungpook National University.