An analysis of the effects of the income level of the family caregivers for the recipients in long-term care facilities on the willingness to pay for use of better services: A cross-sectional study
Article information
Abstract
Purpose
The purpose of this study is to confirm how the income level of the family caregivers for recipients in long-term care (LTC) facilities are related to family caregivers’ willingness to pay out-of-pocket payments for better LTC services.
Methods
This study used the 2021 survey data on cost sharing in LTC facilities, which surveyed 1,111 family caregivers of recipients. To analyze the effect of the income level of family caregivers on the willingness to pay out-of-pocket payments for better LTC services, a chi-square test, a Cochran-Mantel-Haenszel test, and a logistic regression analysis were performed.
Results
We found that 39.0% of respondents were willing to pay out-of-pocket payments if better services were available to recipients. Adjusted for recipient’s and family caregivers’ variables, characteristics of out-of-pocket payment, and LTC service use, the willingness to pay in the monthly household income level of 5 million won and more was 3.28 times higher than those in the monthly household income level of less than 1 million won (95% confidence level=1.93~5.55, p<.001). As monthly household income rises, the odds ratio of willingness to pay tended to increase (p<.001).
Conclusion
Family caregivers who bear the out-of-pocket payments of LTC facilities are willing to pay more for better LTC services. In addition, the higher the income level of family caregivers, the higher their willingness to pay. A full-scale review of the system reform is needed to prevent out-of-pocket payments from becoming an economic barrier to service users and to contribute to service quality improvement and financial stability.
INTRODUCTION
1. Necessity of Study
The long-term care (LTC) insurance system for the elderly was first introduced in July 2008, so the Korean government could bear the burden of caring for older adults. This system is based on the principle of social solidarity, and the system has remained a key service for the care of older adults for the past 15 years with high national satisfaction [1]. As Korea’s population is rapidly aging with the first baby boomer generation (born between 1955 and 1963) entering older adult population in 2020, the characteristics of the older population are also expected to change [2]; therefore, the LTC insurance is faced with the challenge of simultaneously (a) ensuring the sustainability of the insurance system in preparation for increased demand for LTC and (b) achieving institutional reforms that reflect the characteristics of the new elderly generation over the next 15 years. The baby boomer population, who are different from the current older adult population, had higher education and income; thus, new services and better quality of services are required for them [3-5]. In addition, the results of the national surveys presented that most older people would like to live in LTC facilities with their spouses when they need LTC [3,6]. The results have become arousing much interest among Korean people leading to the introduction of new services and improvements in the quality of facility care (i.e., LTC) [7].
Grade 1 or 2 recipients who need significant assistance or rely entirely on others can use the institutional care benefits in their daily life. Exceptionally, Grade 3 to 5 recipients may also use these benefits after getting approval from the Assessment Committee if they have severe behavioral problems caused by dementia. LTC facility benefits are to provide assistance for physical activities, education, and training support, and improve the mental and physical functions of older adults admitted in LTC facilities [8]. As of December 2021, 23.9% of the 789,522 beneficiaries used institutional care benefits, and most of the institutional care beneficiaries (91.7%) are using nursing facilities for older adults [9]. The out-of-pocket payments of the LTC insurance for the elderly refer to the costs borne by the recipients or their family members who directly benefit from LTC services, and recipients who use institutional care benefits must pay their out-of-pocket payments based on their LTC grades and income levels. According to a study by Kwon et al. [4], the average out-of-pocket payment given to LTC facilities was 587,417 won per month as of March 2021.
Resource input is an imperative requirement to introduce new services to LTC facilities and improve service quality in this setting [10]. Out-of-pocket payments that increase commensurately with this can act as a barrier to use the service. Therefore, before discussing the introduction of new services and improvement of service quality in LTC insurance, the willingness to pay out-of-pocket payments should be considered first to confirm their acceptability of the system improvement [11]. The willingness to pay is defined as the consumer’s willingness to pay for the current or improved state of a specific environment, and is a concept used to measure the benefits arising from a new service when it is introduced [12,13].
The results of the LTC insurance service satisfaction in 2021 [1] showed that the demands for improving the service quality in LTC facilities and the burden of service expenses co-existed, as shown in the demands of the survey respondents, such as “Reducing the economic burden of recipients by expanding the number of recipients eligible for a reduction of out-of-pocket payments (48.8%),” “Expansion of LTC service recipients so that more older recipients can benefit from the service (38.0%),” and “Discovering and providing various services suitable for individuals’ functional status (32.8%).” Based on these results, researchers determined that it is crucial to identify the willingness of the family caregivers (cost bearers) to pay out-of-pocket payments for use of better services in LTC facilities. In particular, considering that the income level of recipients and their families’ acts as a major factor in determining the type and quantity of services [14] as well as the amount of out-of-pocket payments [15], it is necessary to closely examine the differences in the willingness to pay more for better services in each income level and how the income level affects one’s willingness to pay.
Few studies have examined recipients’ or families’ willingness to pay out-of-pocket payments for services in LTC facilities. Lee et al. [12] and Lee and Lee [13], which were conducted before the introduction of LTC insurance, estimated the total value of LTC insurance by using the amount of out-of-pocket payments that recipients were willingness to pay when LTC insurance was introduced as a form of social insurance in Korea. Kim et al. [11] examined the needs and the willingness to pay for oral hygiene services for home care benefit recipients. The studies regarding out-of-pocket payments for LTC institutional care examined the actual status of out-of-pocket payments in LTC facilities [4,16] and the relationship between out-of-pocket payments and income levels [15]. Yet, studies that examined the willingness to pay out-of-pocket payments for services in LTC facilities by income levels are still lacking. Thus, this is the time to conduct research on the willingness to pay out-of-pocket payments by each income level.
2. Study Purpose
The study aimed to examine how the income level of the recipients in LTC facilities affects their willingness to pay out-of-pocket payments for better LTC services. The specific aims were to analyze the income level of the family caregivers (cost bearers) and general characteristics of recipients and family caregivers according to their willingness to pay out-of-pocket payments; explore the difference in willingness to pay out-of-pocket payments according to the income level before and after adjusting the characteristics of the out-of-pocket payments and LTC service use; and examine the effect of the income level on the willingness to pay out-of-pocket payments.
METHODS
Ethics statement: This study was approved by the Institutional Review Board (IRB) of National Health Insurance Service (IRB No. 연-2021-HR-01-027). Informed consent was obtained from the participants.
1. Study Design
We conducted a descriptive study to examine the effect of income level of the family caregivers who pay out-of-pocket payments for recipients in LTC facilities on their willingness to pay out-of-pocket payments for use of better services.
2. Study Participants
The study participants were family caregivers of institutional care recipients in March 2021 who completed the 2021 survey on cost sharing in LTC Insurance. Of 123,578 institutional care benefit users identified as of March 2021, 1,231 users were selected for the survey using the proportional stratified sampling method in consideration of the following stratification variables: LTC grades (Grade 1 [accreditation score≥95 points], Grade 2 [75 points≤accreditation score<95 points], Grade 3 [60 points≤accredited score<75 points], Grade 4 [51 points≤accredited score<60 points], Grade 5 [45 points≤accredited score<51 points]), eligibility for health insurance subscribers (general, reduced benefit recipients, medical aid beneficiaries), region where the LTC facility is located (large city, small/medium city), entity of facility establishment (individual, corporation, local government), and number of facility employees (<10, ≥10, <30, ≥30, <100, ≥100). The survey was completed by reflecting ±2.97% at the 95% confidence interval (CI). In this study, we analyzed data from family caregivers of 1,111 LTC institutional care recipients.
3. Study Data
We analyzed data from the survey on cost sharing in LTC insurance [4] conducted by the Health Insurance Research Institute of the National Health Insurance Service. The survey was commissioned to a specialized institution and conducted in the form of a phone or web survey from June 7 to August 7, 2021.
4. Data Analysis
The general characteristics according to the distribution of the monthly household income level and family caregivers’ willingness to pay out-of-pocket payments were confirmed by conducting descriptive statistical analysis and frequency and percentage analysis. We calculated the monthly household income based on the March health insurance premium of individuals certified for LTC insurance in 2021, and confirmed that the 5th quintile distribution of the income was the same as the monthly income distribution of households in the survey. The monthly household income was classified into four levels: “less than 1 million won,” “greater than or equal to 1 million won and less than 3 million won,” “greater than or equal to 3 million won and less than 5 million won,” and “greater than or equal to 5 million won.” We conducted a chi-square test to confirm the difference in the willingness to pay out-of-pocket payments according to the monthly household income of the family caregivers. The Cochran-Mantel-Haenszel test was also conducted to confirm such difference after adjusting the characteristics of the out-of-pocket payments (level of non-benefit out-of-pocket payments, financial burden of out-of-pocket payments) and the characteristics of LTC service use (satisfaction with service quality, need for quality improvement). Then, we performed a logistic regression analysis to examine the effect of family caregivers’ monthly household income on their willingness to pay out-of-pocket payments for use of better LTC services. With logistic regression, we presented three models which used the demographic characteristics of the recipients and the family caregivers and characteristics of out-of-pocket payments and LTC service use as controlled variables, as these variables affect the monthly household income level of the family caregivers. The “less than 1 million” group was set as a reference group, and the odds ratios were obtained to analyze the effect on the willingness to pay out-of-pocket payments. Moreover, we conducted Hosmer and Lemeshow tests to evaluate the goodness of fit of the models, and calculated and analyzed -2 log likelihood values to compare the goodness of fit between models. Additionally, we analyzed the ‘p for trend’ value of logistic regression to identify the tendency for increased or reduced willingness to pay out-of-pocket payments as the monthly household income level increases. SAS ver. 9.4 (SAS Institute Inc.) was used for all statistical analyses conducted in this study.
5. Ethical Considerations
This study was conducted after receiving approval (연-2021-HR-01-027) from the IRB of the Health Insurance Research Institute of the National Health Insurance Service. After explaining the purpose and contents of the survey, participants gave consent to participate in the survey. Data analysis was conducted after de-identifications of personal information.
RESULTS
1. General Characteristics of the Recipients and Family Caregivers by Income Level and Willingness to Pay
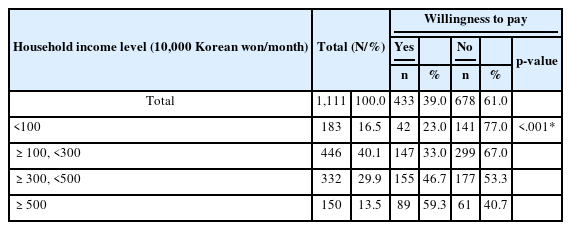
In the distribution of income levels and willingness to pay, the survey respondents who had an income level of “more than 1 million won and less than 3 million won” accounted for the greatest percentage at 40.1%, and those who were willing to pay more accounted for 39.0%. The results of analyzing the demographic characteristics of the survey respondents by the distribution of income level and willingness to pay are as follows (Table 1).
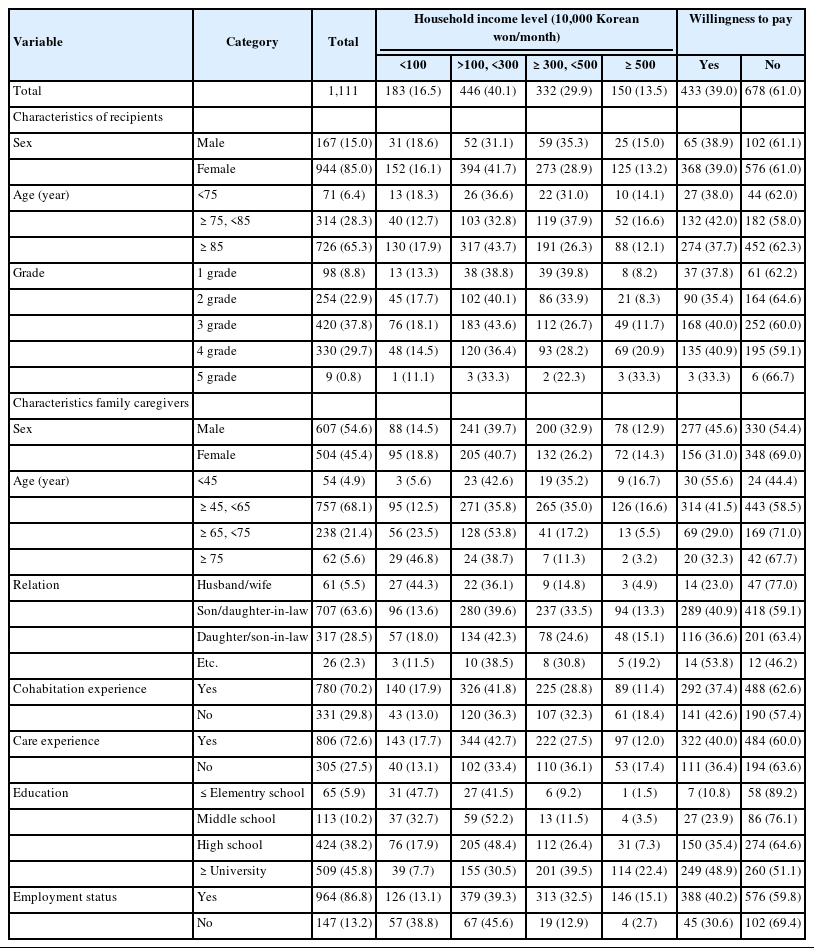
Distribution of General Information, Income Level and Willingness to Pay’s Characteristic of Recipients, Family Caregivers (N=1,111)
First, males with the income level of “more than 3 million won and less than 5 million won” accounted for the highest percentage at 35.3%, and females with the income level of “more than 1 million won and less than 3 million won” accounted for highest percentage at 41.8% in the sociodemographic characteristics of recipients by income level. In terms of age group, 36.6% of those aged 75 or younger and 43.7% of those aged 85 or older had the income level of “more than 1 million won and or less than 3 million won,” and those aged older than 75 and younger than 85 in the income level of “more than 3 million won and less than 5 million won” accounted for the highest percentage at 37.9%. In terms of LTC grade, except Grade 1, 40.1% of Grade 2, 43.6% of Grade 3, 36.4% of Grade 4, and 33.3% of Grade 5 had the income level of “more than 1 million won and or less 3 million won,” accounting for the highest percentage. Male (39.7%) and female family caregivers (40.7%) in the income level of “more than 1 million won and less than 3 million won” accounted for the highest percentage. In terms of age, those under 45, those aged between 45 and 65, and those aged between 65 and 75 in the income level of “more than 1 million won and less than 3 million won” accounted for the highest percentage at 42.6%, 35.8%, and 53.8%, respectively, and those aged 75 or older in the income level of “less than 1 million won” accounted for the highest percentage at 46.8%. Regarding the relationship with the recipients, spouse accounted for the highest percentage at 44.3% in the income level of “less than 1 million won,” and son or daughter-in-law and daughter or son-in-law accounted for the highest percentage at 39.6% and 42.3%, respectively, in the income level of “more than 1 million won and less than 3 million won.” In terms of education level, those who graduated from elementary schools or lower accounted for 47.7% in the income level of “less than 1 million,” and those who graduated from middle school and high school accounted for 52.2% and 48.4%, respectively, in the income level of “more than 1 million won and less than 3 million won.” Those who graduated from universities accounted for the highest percentage at 39.5% in the income level of “more than 3 million and less than 5 million won.”
The demographic characteristics of recipients and family caregivers by the willingness to pay were examined. First, in terms of demographic characteristics of recipients, females (39.0%) were slightly higher than male (38.9%) in their willingness to pay more, and those aged between 75 and 85 accounted for the highest percentage at 42.0%, followed by those under 75 at 38.0% and those aged 85 or older at 37.7%. Those in Grade 4 accounted for the highest percentage at 40.9%. In terms of demographic characteristics of family caregivers with the willingness to pay, males (45.6%) had a higher percentage than females (31.0%), and those aged under 45 accounted for the highest percentage at 55.6%, followed by those aged between 45 and 65 at 41.5%, those aged 75 or older at 32.3%, and those aged between 65 and 75 at 29.0%. In terms of the relationship with the recipient, sons-in-law and daughters-in-law showed the highest willingness to pay more at 40.9%, and those who had no experience living with the recipients accounted for 42.6% and those with experience caring for the recipient accounted for 40.0% in their willingness to pay. Moreover, those who graduated from university or higher accounted for 48.9% of their willingness to pay, followed by high school graduates at 35.4%, middle school graduates at 23.9%, and those who graduated from elementary school or lower at 10.8%. Finally, family caregivers with jobs (40.2%) showed a higher willingness to pay than those without jobs (30.6%).
2. Differences in the Willingness to Pay According to the Income Level of Family Caregivers
Table 2 presents the difference in the willingness to pay out-of-pocket payments according to the income level of family caregivers. When the monthly household income of the family caregivers increases, the participants were more willing to pay out-of-pocket payments for better services. Of those whose monthly household income was “less than 1 million won,” 23.0% were willing to pay. For those whose monthly household income was “greater than or equal to 3 million won and less than 5 million won,” 46.7% were willing to pay more, showing a statistically significant difference (p<.001). However, those who had no willingness to pay accounted for 77.0% in the household income of “less than 1 million won,” but the ratio decreased to 40.7% in the household income of “greater than or equal to 5 million won” (p<.001).
3. Differences in the Willingness to Pay According to the Income Level of Family Caregivers After Adjusting the Characteristics of Out-of-Pocket Payments
Table 3 shows the differences in the willingness to pay out-of-pocket payments according to the income level of family caregivers after adjusting the characteristics of out-of-pocket payments (i.e., the level of non-benefit cost, financial burden). The differences in willingness to pay according to the income level of the family caregivers were statistically significant (p<.001) even after adjusting the level of non-benefit cost. When the level of non- benefit cost was low, 20.3% of family caregivers from the “less than 1 million won” monthly household income were willing to pay more. As their monthly household income increased, their willingness to pay increased to 62.8% when their monthly household income was “more than 5 million won.” When the level of non-benefit cost was high, 34.3% were willing to pay more when their monthly household income was “less than 1 million won,” but it increased to 52.1% when their monthly household income was “more than 5 million won,” showing a statistically significant difference.

Differences in the WTP According to Income Level After Adjusted by Financial Burden of Out-of-Pocket Payment (N=1,111)
Even after adjusting the financial burden of out-of-pocket payments, the willingness to pay out-of-pocket payments increased with statistical significance as the monthly household income increased. When the family caregivers had the financial burden of out-of-pocket payments, only 12.7% were willing to pay more if their monthly household income was “less than 1 million won.” As their monthly household income increased, the caregivers’ willingness to pay more also increased, and it was the highest at 36.6% when their monthly household income was “more than 3 million won and less than 5 million won.” Even when they had no financial burden of out-of-pocket payments, 41.5% were willing to pay if their monthly household income was “less than 1 million won.” As their monthly household income increased, their willingness to pay out-of-pocket payments also increased; particularly, 79.5% were willing to pay when their monthly household income was “more than 5 million won.”
4. Difference in the Willingness to Pay According to the Income Level of Family Caregivers After Adjusting the Characteristics of LTC Service Use
Table 4 shows the difference in the willingness to pay according to the income level of the family caregivers after adjusting the characteristics of LTC service use (i.e., satisfaction with service quality, need for quality improvement). There was a significant difference in the willingness to pay according to the income level of family caregivers after adjusting the characteristics of LTC service use (p<.001). When the family caregivers were dissatisfied with the quality of LTC services, 16.7% of them were willing to pay if their monthly household income was “less than 1 million won.” As they had a higher monthly household income, their willingness to pay also increased; particularly, 43.4% were willing to pay when their monthly household income was “greater than or equal to 3 million won and less than 5 million won.” Even when the family caregivers were satisfied with the quality of LTC services, 25.2% of them had the willingness to pay more if their monthly household income was “less than 1 million won.” As they had a higher monthly household income, their willingness to pay also increased; 65.0% were willing to pay when their monthly household income was “more than 5 million won.”

Differences in the WTP According to Income Level After Adjusted by Characteristics of Long-Term Care Service Use (N=1,111)
When the improvement in the quality of LTC services was adjusted, there was a statistically significant difference in willingness to pay according to monthly household income. In the group that felt that service quality improvement was unnecessary, the willingness to pay increased as their monthly household income increased. The willingness to pay was 18.6% in the monthly household income of “less than 1 million won,” but it increased to 23.6% in the monthly household income of “greater than or equal to 1 million won and less than 3 million won,” 34.5% in the monthly household income of “greater than or equal to 3 million won and less than 5 million won,” and 52.4% in the monthly household income of “greater than or equal to 5 million won.” Even in the group that felt the service quality needed to be improved, the willingness to pay increased according to the income level. The willingness to pay was 32.2% in the monthly household income of “less than 1 million won,” but it increased with statistical significance to 64.4% in the monthly household income of “greater than or equal to 5 million won.”
5. The Effect of the Income Level of the Family Caregivers on the Willingness to Pay Out-of-Pocket Payments
Table 5 presents the results of logistic regression analyses to identify the factors influencing the willingness to pay out-of-pocket payments for use of better services. In the analysis, Models 1, 2, and 3 were constructed and analyzed by adding controlled variables, which are factors influencing the willingness to pay. Model 1 analyzed the effect on the willingness to pay using only the monthly household income variable without adjusting other influencing factors. The Hosmer and Lemeshow test results showed that the model was appropriate (p=1.000). Specifically, the willingness to pay out-of-pocket payments was 4.90 times higher (95% CI=3.05~7.87) when the monthly household income was “greater than or equal to 5 million won” than when it was “less than 1 million won.”
Model 2 adjusted the general characteristics of the recipients (i.e., sex, age, grade), the family caregivers (i.e., sex, age, relationship with the recipient, experience living with the recipient, care experience, education level, jobs). The model’s goodness of fit test showed that the model was appropriate (p=.999). The analysis results showed that compared to the monthly household income of “less than 1 million won,” the willingness to pay out-of-pocket payments was 2.17 times higher (95% CI=1.40~3.38) when the monthly household income was “greater than or equal to 3 million won and less than 5 million won” and 3.64 times higher (95% CI=2.18~6.09) when the monthly household income was “greater than or equal to 5 million won.”
Model 3 adjusted the general characteristics of the recipients and the family caregivers, the characteristics of out-of-pocket payments (i.e., level of non-benefit cost, financial burden of out-of-pocket payments), and the characteristics of LTC service use (i.e., satisfaction with service quality, need for quality improvement). The Hosmer and Lemeshow test results showed that the model goodness of fit was statistically significant (p=.928). The analysis yielded that the odds of family caregivers willing to pay out-of-pocket payments for use of better services was 3.28 times (95% CI=1.93~5.55) higher when their monthly household income was “greater than or equal to 5 million won” than when it was “less than 1 million.” In addition, as a result of analyzing the tendency for the odds ratio of willingness to pay, the willingness to pay tended to increase as the monthly household income increases in all three models (p<.001).
DISCUSSION
This study examined the effect of family caregivers’ income level on their willingness to pay out-of-pocket payments for use of better LTC services for institutional care recipients. As a result, 39.0% of the participants were willing to pay out-of-pocket payments if a recipient could use a better service than the current one. Specifically, 46.7% of those with a monthly household income of “greater than or equal to 3 million won and less than 5 million won” and 59.3% of those with the monthly household income of “greater than or equal to 5 million won” showed the willingness to pay out-of-pocket payments. The results indicate that those with higher monthly household incomes are more willing to pay out-of-pocket payments. In addition, the willingness to pay out-of-pocket payments increased in the group paying high non-benefit out-of-pocket payments and in the group feeling no financial burden of the out-of-pocket payments and having a high monthly household income. It was also confirmed that as the monthly household income of the family caregivers increased, the willingness to pay out-of-pocket payments significantly increased, even after adjusting demographic characteristics of recipients and family caregivers, non-benefit out-of-pocket payments, the financial burden for out-of-pocket payments, satisfaction with service quality, and need for quality improvement.
The family caregivers’ financial and education levels are key contributors to choosing the types of services and the use of LTC services. Brau and Lippi Bruni [17] suggested that coverage of LTC service is lower in the lower-income class than in the other classes, and that income influences the service purchase power. In domestic studies, the amount of benefit use was relatively low in the low-income class in a low health insurance premium quintile [18], and the income level had a significant effect on the choice of facility admission and the amount of home care service use [14].
The financial resources required for the operation of LTC insurance consist of the national treasury, insurance premiums, and out-of-pocket payments paid by the users. The results of our study showed that the higher the monthly household income, the higher the recipient’s willingness to pay more out-of-pocket payments if it resulted in better services. These results are consistent with the results of studies conducted in Germany [19] and Taiwan [20] on the willingness to pay health insurance premiums and LTC insurance premiums for older adults. In a study conducted in Germany [19], the recipients were asked, “Assuming that you have no health insurance, how much health insurance premium per month are you willing to pay if the current level of health insurance service is provided, considering your income level?” The result was that the higher their income level, the higher the amount they could pay. In a study conducted in Taiwan that examined the willingness to pay the insurance premiums required to continue health insurance services and expand their scope to LTC [20], it was also found that the higher the household income, the higher the willingness to pay and the higher the amount that could be paid. Through these two studies, the household income of the family caregivers correlates with their willingness to pay insurance premiums and the amount they can pay, which indicates that the income of family caregivers is a variable that significantly affects (a) the willingness to pay for the maintenance, continuation, and expansion of social insurance and (b) the amount they can pay.
In addition, Japan’s LTC insurance system applies the out-of-pocket payment rate differentially according to the user’s ability to pay to secure the system’s financial sustainability [4,21]. In the early stage of the system introduction in April 2000, the out-of-pocket rate of 10% was applied uniformly, but 20% (from August 2015) or 30% (from August 2018) was applied differentially to the high-income class later [4]. The impact of the 20% increase included a decrease or increase in service use or suspension of the service between the 10% and 20% groups, but it was not statistically significant [21]. In addition, after the 30% increase in the out-of-pocket payment rate, the rate of decrease or suspension of the use of LTC services was 3.2% in the 20% group and 5.2% in the 30% group. The rate was higher in the 30% group, but a statistical verification was not conducted. These two surveys presented that the increase in the out-of-pocket payment rate had statistically minimal effect on the amount of care service used.
LTC service users consider the mitigation of out-of-pocket payments (41.3% in 2019, 49.9% in 2020, and 48.8% in 2021) as the most important thing for system improvement [1]. However, it should be noted that, as seen in the results of our study, as much as 39.0% of the service users said they would pay more out-of-pocket payments than now if they could use better services. This indicates that it is necessary to have an institutional mechanism where the mitigation of out-of-pocket payments is expanded and high-quality services are available to those who want to pay more out-of-pocket payments.
The willingness to pay out-of-pocket payments should have a precondition that recipients could use better services. Better LTC institutional service and “good care” can be defined in various ways depending on the characteristics of the defining entities and the environment surrounding them. Seok [10] defined “good care” as living like a human until the day of death while sustaining the remaining ability to the maximum in a safe environment, holding the right to self-determination under professional judgment, considering individual tastes, and maintaining relationships with family members. In other words, person-centered service rather than provider-centered service can be defined as good care. Murphy [22] conducted a survey targeting the nurses who provided LTC services and concluded that the factors that influence “good care” include services that increase the independence and autonomy of users and create a home-like environment, along with person-centered services that increase intimacy and professional services by experienced and competent staff. Additionally, staff must have a strong understanding of users’ conditions and desires. The results of these two studies indicate that to enjoy “good care,” the recipients should be able to (a) use professional services by staff who are well aware of the various conditions and needs of recipients in a safe and comfortable environment and (b) live a dignified life while actively interacting with their families or local communities. To provide such good care, we need to invest in infrastructure aspects, such as providing more private bedrooms to guarantee personal privacy and control infectious diseases, strengthening manpower allocation standards to provide more direct services, and securing more diverse and professional service providers [23]. The area that accounts for the highest percentage of LTC insurance benefit costs (fee) is labor costs [24], so adjustment of the fee schedule should also be considered in this discussion.
The cost bearers (family caregivers) unanimously emphasized that the “medical and nursing services” must be improved within the LTC facilities. In a survey about LTC in 2019, 6.9% of the survey respondents were not satisfied with the LTC facilities’ nursing and medical services, and 16.2% of respondents reported that the treatment service specialized for diseases must be improved in institutional care benefits [5]. Part-time doctors, nurses, or nursing assistants are providing medical and nursing services in LTC facilities. It is prescribed in the law that at least one part-time doctor should be assigned to a LTC facility, and one nurse or nursing assistant should be assigned to 25 residents [8]. According to the LTC benefit provision standards, institutional care benefit institutions, including LTC facilities, should assign nurses preferentially to manage the health of residents [25]. However, as of the end of December 2021, nurses accounted for only 14.4% of the whole nursing staff (nurses and nursing assistants) in institutional care benefit institutions, including LTC facilities [9]. It was found that 6.5% of LTC facility users (112,741 as of April 2016) experienced hospitalization, and 82.7% received outpatient medical treatment [26]. The most frequent diseases for either hospitalizations or outpatient medical treatments were unspecified pneumonia, Alzheimer’s dementia, essential hypertension, and cerebral infarction. The residents in LTC facilities have a high level of medical and nursing care needs. Therefore, in order for them to actively respond to the medical and nursing services provided by LTC facilities, it is necessary to have a full-fledged discussion on medical and nursing services provided in LTC facilities as well as strengthen the nurse staffing standards.
Lee et al. [6] found that a new group of older adults with a higher education level, higher income, and higher financial independence than the current older adult population had appeared. When this new group of older adults use LTC services, they will demand more specialized, diverse, and personalized services than they receive now. Thus, the LTC insurance system should be improved to meet this new group’s expectations and to consider their financial sustainability. For future implications, it is necessary to think more deeply about a system that can actively respond to optional services to reflect individual preferences and improve the quality of basic care services. In Germany, Article 88 of the LTC Insurance Act stipulates that additional benefits can be provided to older residents under the agreement with older adults beyond the necessary LTC services. These additional benefits refer to particularly good services related to care, meals, and additional caregiving services, which are made under the agreement between older adult resident and the LTC facility. In principle, the entire cost shall be borne by the users [4].
From the standpoint of older adults in a LTC facility, the facility is both residential and living space. Therefore, it is necessary to devise a plan that can address the individual and diverse needs of older adults residing in LTC facilities. In a study by Kwon et al. [27], both academic and field experts agreed on the provision of additional services to the recipients, such as additional cognitive activities at the request of recipients, a physical function recovery program, and individual meals at a time and place desired by recipients, at a cost that exceeds the current out-of-pocket payment rate. However, there is still no discussion on essential care services in LTC insurance. Based on our findings, we recommend a system that can provide optional services beyond the scope of mandatory standards or basic care services. In addition, a cost burden mitigation policy should also be discussed to prevent the recipients from being unable to properly use necessary services due to financial burdens.
In this study, we found that 39.0% of recipients were willing to pay more out-of-pocket payments for the use of better services. To our knowledge, this study is the first study to examine the effect of the monthly household income of the family caregivers and their willingness to pay out-of-pocket payments for the use of better LTC services.
However, this study has some limitations. First, the monthly household income value may differ from the actual household income because the survey respondents subjectively reported their income values. We converted the monthly household income based on the March health insurance premium of the certified LTC recipients in 2021 of the households that the survey respondents found to be the same as the 5th quintile distribution. Second, this study targeted only the cost-bearers (family caregivers) for institutional care benefit users. Institutional care benefits and home care benefits have differences in non-benefit expenses, such as meal material cost and out-of-cost expense rate (institutional care benefit: 20% of benefit cost, home care benefit: 15% of benefit cost), but this study analyzed only the institutional care benefits. Therefore, it is necessary to analyze the willingness to pay out-of-pocket payments for each income level of the cost-bearers (family caregivers) paying the cost of home care benefits in the future. Third, in this study, the cost bearers were composed of only family members who were paying out-of-pocket payments. In Korea, most of the out-of-pocket payments for LTC facilities are paid by the older person’s adult children. The proportion of paying partial or full out-of-pocket payments has increased from 1.8% [16] in 2010 to 9.4% [28] in 2021, but the proportion of family members, such as children, paying the cost of LTC service is still higher than that of recipients themselves. As the proportion of recipients of pensions such as private pensions and basic pensions is increasing, the proportion of recipients paying the cost of LTC services is expected to gradually increase. Lee et al. [29] suggested that a “new elderly generation” with significantly different characteristics and needs from the current older adults has emerged. Lee et al. [29] argued that this generation will show characteristics that are different from the previous elderly generations in various ways, such as a high level of education, familiarity with leisure culture, and a high desire to participate. Han [30] examined the requirements of the new older generation for LTC services. They found that the new older generation had high requirements for personal health care, respect for lifestyle, social interaction, high quality of service, and a safe environment. Lee et al. [29] and Han [30] suggested that post-baby boomers have high secondary education completion rates, high income levels, and diverse personalities and needs. In other words, the consumers who will use LTC services in the future need to deeply consider how they will respond to their various needs and expectations for high quality services. For future implications, tailoring a fact-finding survey to this emerging baby boomer generation and conducting a follow-up study to identify the service quality that they want and their perception of the cost burden regarding LTC services and facilities are recommended.
CONCLUSION
In the LTC insurance system, out-of-pocket payments are one of the main sources along with LTC insurance premiums and national and local government contributions. In this study, 39.0% of the families of LTC institutional care recipients were willing to pay out-of-pocket payments if older adults can use better LTC services. As the income level of the cost-bearers (family caregivers) increased, their willingness to pay out-of-pocket payments also increased. Our findings indicate that the review of the out-of-pocket payment system should be discussed along with the review of the quality of LTC services. It is necessary to reach a social consensus by publicizing the LTC services the family caregivers want, how much more they can pay for better services, and how much more they are willing for LTC insurance premiums. A full-scale review of the system reform is necessary to prevent out-of-pocket payments from becoming an economic barrier to service use and to allow the out-of-pocket payments to contribute to service quality improvement and financial stabilization of the LTC insurance system for older adults.
Notes
Authors' contribution
Study conception and design acquisition - JK and EJH; Data collection - HKK; Analysis and interpretation of the data - EJH and HKK; Drafting and critical revision of the manuscript - JK, EJH, and HKK; Final approval - JK and EJH
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Supplementary materials
Further details on supplementary materials are presented online (available at https://doi.org/10.17079/jkgn.2212.20001).