Relationships between health literacy, self-efficacy, and medication adherence in older people with polypharmacy: A cross-sectional study
Article information
Abstract
Purpose
This study identified the relationships between health literacy, self-efficacy, and medication adherence among older people with polypharmacy and analyzed the factors affecting medication adherence.
Methods
This was a cross-sectional study using a survey of 95 participants who were on five or more drugs, 65 years or older, and visited one community center in Seoul between August 5, 2019 and August 7, 2019. Data were collected using a questionnaire and analyzed with descriptive statistics, t-test, ANOVA, Tukey test, Pearson's correlation coefficient, and multiple regression via the IBM SPSS 23.0 program.
Results
The participants took on average 8.32±3.90 drugs daily. Their health literacy was very low at 3.53±2.07. Self-efficacy and medication adherence were high at 33.63±5.36 and 15.03±3.27, respectively. Health literacy differed based on age and education levels, whereas self-efficacy differed depending on the frequency of medication. No demographic or medication-related factors caused a difference in medication adherence. Health literacy did not correlate with self-efficacy and medication adherence. Self-efficacy showed a negative correlation with medication adherence (r=-.52, p<.001). However, as a lower medication adherence score indicates greater adherence, a negative correlation means higher self-efficacy is linked with better adherence. Self-efficacy influenced medication adherence (β=-0.52, p<.001) with an explanatory power of 27.0% (F=17.01, p<.001) in this group. Also, the negative regression coefficient means higher self-efficacy was associated with better adherence.
Conclusion
Medication adherence was generally high, with self-efficacy being the main influencing factor. Hence, intervention programs that promote self-efficacy should be implemented for older people with polypharmacy.
INTRODUCTION
1. Necessity of Study
The prevalence of chronic diseases in older people is increasing due to aging and heightened susceptibility to diseases, which accelerates the administration of medication to manage such diseases. This leads to polypharmacy in older people, whereby consumption of 10 or more medication among the chronically ill is not uncommon [1]. Generally, polypharmacy refers to taking more than five medication daily [2]. A study on polypharmacy cases must take into consideration not just prescription drugs but also non-prescription drugs that patients can readily purchase without prescriptions [3]. This may be because polypharmacy heightens the possibilities of drug-drug interaction and adverse drug reaction which are harmful unintended consequences caused by taking multiple medication [4], and may induce negative health outcomes for older people [5].
Chronic diseases in older people frequently require adequate lifestyle maintenance and consistent medication adherence to manage and alleviate symptoms. However, previous research has revealed that 54.2% of hypertensive patients showed low medication adherence [6]. Poor adherence may result in disease deterioration and failure of treatment [6]. Although the rate of polypharmacy is steadily increasing [7], current studies in Korea are limited to studying drug usage [8]. A systematic review of international research revealed a lack of investigation into medication adherence among older people with polypharmacy [9]. Adequate medication adherence is especially important in older people with chronic illnesses as these patients consume a large number of drugs. Hence, it is necessary to ascertain factors related to medication adherence among chronically ill older people with polypharmacy.
Factors affecting medication adherence are complex and diverse [6]. They include demography, health-related factors, cognitive ability, psychosociological factors, and medication-related factors in addition to health literacy and self-efficacy [10,11]. Health literacy, the ability to obtain and comprehend basic information and services required for health management and undertake relevant actions in daily life, is imperative to conduct health behavior [12]. According to previous research [10], health literacy and medication adherence of the older people showed a positive correlation, and health literacy was identified as a factor influencing medication adherence. At the same time, previous research [5] showed that polypharmacy and cognitive function had a negative association. Hence, it is necessary to identify the effect of polypharmacy on health literacy. In addition, medication adherence may be complicated by many factors such as the exact dosage, frequency, timing, and route of intake. Therefore, it is necessary to investigate the effect that health literacy has on medication adherence in older people with polypharmacy. However, previous research in Korea regarding health literacy is mainly focused on the introduction of concepts and the development of study tools [13], which has led to a lack of research regarding the effect that health literacy has on medication adherence of older people with polypharmacy. Hence, there is a need to identify the extent of health literacy in older people with polypharmacy and the effect it has on medication adherence.
Self-efficacy, defined as confidence in one’s ability to adequately perform the requisite tasks on hand, is an important concept in explaining medication adherence [14]. This is because behavioral change or adherence is a significant area of concern in nursing. According to previous research, an influential variable in explaining the medication adherence of chronically ill outpatients is self-efficacy [11]. As failure to abide by one’s medication regimen may complicate the success of the treatment [14], it is important to understand the self-efficacy of older people with polypharmacy. However, since current research has focused mainly on the effectiveness of interventions designed to improve self-efficacy [15], there is a lack of research on self-efficacy of chronically ill older people with polypharmacy. Hence, it is necessary to identify the extent of self-efficacy in older people with polypharmacy and its relationship with medication adherence.
Therefore, the relationships between health literacy, self-efficacy, and medication adherence in the older people with polypharmacy and the effect of health literacy and self-efficacy on medication adherence should be established.
2. Study Purpose
This study aims to investigate the relationships between health literacy, self-efficacy, and medication adherence in older people with polypharmacy and provides information for developing interventions that improve medication adherence by identifying the factors that affect it.
METHODS
Ethic statement: This study was approved by the Institutional Review Board (IRB) of Seoul National University (IRB No. 1907/002-012).
1. Study Design
This is a descriptive cross-sectional study that identifies the relationships between health literacy, self-efficacy, and medication adherence of older people with polypharmacy in the community, and the factors that influence medication adherence.
2. Participants
The participants of this study were registered members of one community center located in Seoul. Each participant was 65 years or older, consumed five or more prescription and non-prescription drugs each day [2,3], did not suffer from dementia (indicated by a score of 24 or above on the Mini-Mental State Examination), had no problems communicating, and expressed their comprehension and consent of this study.
The number of subjects required for this study was calculated to be 127. This figure was derived using the G*power 3.1 (Düsseldorf, Germany) with the following specifications: effect size=.15, significance level=.05, power=.8, and predictor variable=12. Considering the disqualification rate, a total of 140 people was surveyed, and barring five incomplete answers, 135 surveys were analyzed.
3. Measurements
1) Demographic and Medication-Related Characteristics
Sex, age, education level, whether a family member lives together, state of perceived health, daily number and type of medications, daily frequency of medication, and past experience with side effect of medication were considered. Questions pertaining to nonprescription drugs were selected based on previous research [16,17].
2) Health Literacy
This study measured health literacy using the eight-question, Short Version of the Korean Functional Health Literacy Test created by Kim [12], which was based on The Test of Functional Health Literacy in Adults created by Baker et al. [18]. There were four questions each on numeracy and reading comprehension. Each correct answer was awarded 1 point, whereas an incorrect answer was allotted 0 points. The score ranged from 0 to 8, with higher scores indicating greater health literacy. The Kuder-Richardson 20 value of the tool was .84 [12] and that of the study was .73.
3) Self-Efficacy
The Self-Efficacy for Appropriate Medication Use Scale, created by Risser et al. [14], was translated into Korean by Kim and Kim [15]. The tool measures participants’ confidence in their medication intake. It comprises 13 questions. The patients were allowed to answer one of the following questions: “very confident” (3), “somewhat confident” (2), and “not confident” (1). The scores range from 13 to 39, with higher scores indicating greater self-efficacy. The Cronbach's α value of the tool was .96 [15] and that in this study was .89.
4) Medication Adherence
The Adherence to Refills and Medication Scale (ARMS), created by Kripalani et al. [19], was translated into Korean (ARMS-K) by Kim et al. [20]. In this study, the ARMS-K was used to measure medication adherence. The survey comprised 12 questions. Eight questions pertained to the frequency of missed medications, examining the subject’s willingness to follow the regimen, and four questions on whether the subject pre-plans before his or her medication runs out, an indication of the subject’s willingness for re-prescription. Each question was answered in one of the following ways: “always not” (1), “sometimes” (2), “frequently” (3), and “always” (4). Question 12 on the survey was reverse-coded during the analysis. The scores ranged from 12 to 48, with lower scores indicating greater medication adherence. The Cronbach's α value of the tool was .80 [20] and that of this study was .77.
4. Data Collection
The data for this study was collected from older people with polypharmacy registered at one community center in Seoul, with permission from the director of the community center, after an approval by the IRB. Data were collected by the researcher and three trained research assistants between August 5, 2019 and August 7, 2019. Prior to data collection, each of assistants were trained on how to conduct the data collection in order to ensure standardization.
The subjects were informed of the purpose of this study and gave written consent. Subsequently, the participants completed the survey. Those with decreased sight or those wishing for the survey to be read to them―though not illiterate―had the survey read out to them and assistance was provided as they completed the survey. Participants who completed the survey were compensated with gift cards.
5. Ethical Considerations
The survey was conducted only with willing participants and was approved by the Seoul National University’s IRB (IRB No. 1907/002-012). The collected data were used for research purposes only. Furthermore, the data were anonymized, and the participants were informed of their right to stop the survey at any time. Two copies of the consent form were signed, one of which was provided to the participant.
6. Data Analysis
The collected data were analyzed using the SPSS/WIN 23.0 (IBM Corp.) program. First, the participants’ demographic and medication-related characteristics were examined by using descriptive statistics. Second, health literacy, self-efficacy, and medication adherence were analyzed using mean, standard deviation, and range. Third, the differences in health literacy, self-efficacy, and medication adherence according to the participants demographic and medication-related characteristics were analyzed using the independent t-test or one-way ANOVA and post-hoc Tukey test. Fourth, the Pearson’s correlation coefficient was used to identify the correlation between health literacy, self-efficacy, and medication adherence. Finally, the enter method of multiple regression was used to determine the factors influencing medication adherence.
RESULTS
1. Demographic and Medication-Related Characteristics
Ninety-five participants took five or more prescription drugs and were included in the analysis. Forty additional participants were surveyed but their results were omitted from analysis because their tally of five or more drugs included non-prescription drugs as well as prescription drugs. Seventy-five (78.9%) were male and twenty (21.1%) were female. Their ages ranged from 65 to 94 years, with a mean age of 79.7±6.5. Forty-two (44.2%) responded that they were living alone. Fifty-five participants (57.9%) had completed at least high school education. Sixty-six (69.5%) responded that their health was in at least “moderate” state. The daily number of prescription drugs ranged from 5 to 30, and the mean number of prescription drugs was 7.71±3.90. The daily mean of non-prescribed drugs was 0.62±1.10 and the maximum number was 6. The mean of both prescription and non-prescription drugs was 8.32±3.90 per day. The frequency of drug intake had a mean of 2.25±0.88 and a maximum of five times (Table 1).
2. Levels of Health Literacy, Self-Efficacy, and Medication Adherence
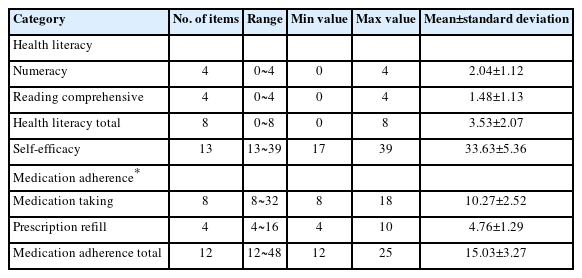
Medication adherence means that the patient takes the medication prescribed by the physician or which is agreed upon by the patient and the physician [21]. The mean medication adherence score of participants taking five or more prescription drugs was 15.03±3.27 from a possible score of 48. The scores for the medication taking and re-prescription sections were 10.27±2.52 from a total of 32, and 4.76±1.29 from a total of 16. The mean health literacy score was 3.53±2.07 out of 8. The scores for the numeracy and reading comprehension section were 2.04±1.12 and 1.48±1.13 out of 4, respectively. Mean self-efficacy score was 33.63±5.36 from a possible score of 39 (Table 2).
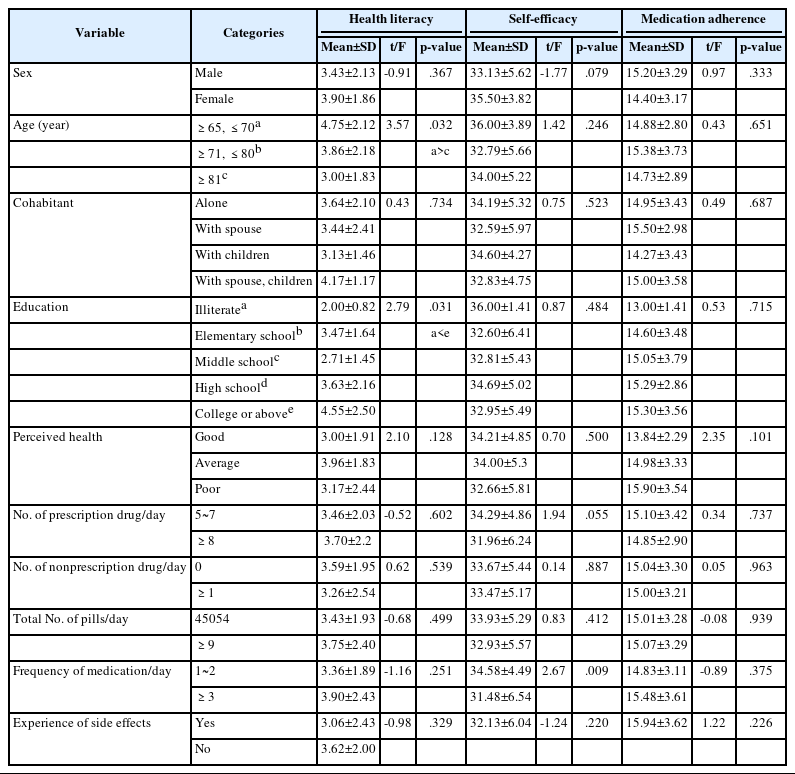
3. Difference in Variables According to Demographic Characteristics
An analysis of the difference in variables according to demographic characteristics revealed that health literacy showed a difference based on age and education levels in participants taking five or more drugs. Health literacy decreased with increasing age (F=3.57, p=.032). Post-hoc analysis showed a difference according to age groups with participants between the ages of 65 and 70 showing a higher level than those over 81. Furthermore, health literacy showed a significant difference according to education levels (F=2.79, p=.031). Post-hoc analysis showed that those with at least college level education had a higher health literacy than those who received no education. An analysis of medication-related characteristics showed that participants who took medication at least three times a day (t=2.67, p=.009) showed a lower level of self-efficacy (Table 3).
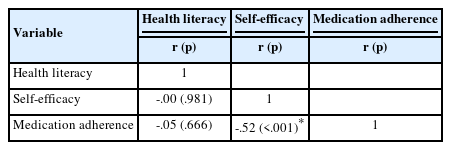
4. Correlation Between Health Literacy, Self-Efficacy, and Medication Adherence
An analysis of the correlation between health literacy, self-efficacy, and medication adherence in participants taking five or more prescription drugs revealed that health literacy did not correlate with self-efficacy or medication adherence. However, self-efficacy had a negative correlation with medication adherence (r=-.52, p<.001) (Table 4). A high score on the scale for self-efficacy indicates a high level of self-efficacy, whereas a low score on the scale for medication adherence indicates a high level of medication adherence. A negative correlation between the two scales ultimately means that as self-efficacy increases, medication adherence will also increase in this study.
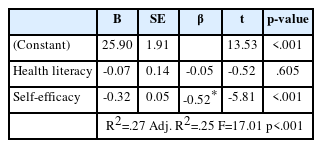
5. Factors That Influence Medication Adherence
To identify the factors that influence medication adherence in older people with polypharmacy, a multiple regression analysis was conducted. There were no demographic and medication-related characteristics that had a significant influence on medication adherence, and hence, these variables were not included in the regression analysis. Medication adherence was designated as the dependent variable, while health literacy and self-efficacy were designated as independent variables in the regression analysis. It was deemed that there was no autocorrelation of the independent variables, as indicated by the Durbin-Watson test result of 1.71, and there was no presence of multicollinearity, as evidenced by a variance inflation factor of less than 10. Self-efficacy was deemed to influence medication adherence (β=-0.52, p<.001) and it had an explanatory power of 27.0% (F=17.01, p<.001) (Table 5). As a low medication adherence score indicates good adherence, a negative regression coefficient means that a higher self-efficacy score indicates better medication adherence.
DISCUSSION
This study provides the basis for the development of nursing interventions that enhance medication adherence in older people with polypharmacy by identifying the relationship between health literacy, self-efficacy, and medication adherence. The participants took a higher number of drugs than those of a previous study [11]. This is probably because the mean age of the participants in this study was higher. Medication intake in older people require attentive care as physiological changes caused by aging may lead to pharmacodynamic alterations in older people [1]. Consequently, it is important to pay attention to non-prescription drugs as well as prescription drugs in older people with polypharmacy [3]. Furthermore, previous research indicates that the combined use of non-prescription drugs along with prescription drugs may lead to a decline in medication adherence [22]. Therefore, in order to achieve the therapeutic objectives, it would be necessary for nurses to educate older people against indiscriminate use of non-prescribed drugs for effective treatment, and for patients to be provided with consultation by a physician.
The participants of this research showed a low level of health literacy, which resulted in a different outcome compared to that of previous research [23]. This is likely because there was a higher percentage of participants aged 81 or above and the mean age of the participants was higher. The participants refused to read longer instructions that required higher levels of comprehension. For instance, during the data collection process, despite the surveyor’s assistance in reading and understanding the meaning of the question regarding colon polypectomy consent in the reading comprehension section, this question yielded the lowest number of correct answers. Polypharmacy has been negatively associated with cognitive function in older people [5], so it can be assumed that they had difficulty understanding some of the longer sentences and instructions in the survey. Therefore, in a clinical setting, it would be more effective to use concise language with visual tools such as images or diagrams than long questionnaires. Meanwhile, the participants of this research showed a higher level of self-efficacy than those of previous research [11]. This may be because a large percentage of them responded that their self-perceived health status was average or above, although the participants of this study were of a higher age. Although the exact sexual distribution and education level were different, a previous study [15] using the same tool showed a lower level of self-efficacy among its participants. This is probably because its participants were orthopedic inpatients. The participants of this study, in contrast, were able to establish social relationships with their peers by enrolling in classes at a local welfare center and were physically active and mobile enough to be able to use public transportation to visit these welfare centers. This most likely contributed to their high level of self-efficacy. Furthermore, the participants’ medication adherence was relatively high, in contrast to previous research on hypertensive individuals [6]. In another study of patients with diabetes mellitus [20], the results were similar to those of this study. It is assumed that the long duration of medication consumption may have contributed to the participants’ conviction regarding appropriate medication consumption. This may have contributed to the high medication adherence. To overcome the limitations of a self-reported survey and obtain an accurate picture of medication adherence, it would be wise to refer to previous research [20] which utilizes objective clinical measurements.
This study revealed that lower age and higher education level were related to higher health literacy, which was similar to previous research [23]. This is likely because younger people can more easily obtain health information from documents or the media and higher education levels make the acquiring of information less difficult. Hence, it seems necessary to consider the age and education levels of the participants when conducting education related to medication intake. Furthermore, self-efficacy according to medication-related characteristics showed a statistically significant difference based on the daily frequency of medication, which was similar to previous research [24]. A higher frequency of medication resulted in lower self-efficacy, which is likely because the negative perception regarding one’s health affects self-efficacy. In this study, there were no variables that showed significant differences in medication adherence according to demographic and medication-related characteristics. However, in previous research, various characteristics of the participants such as sex, education levels [23], experience of side effects [11], perceptions on drug intake [25], and perceived health status [10,22] resulted in differences in medication adherence. Medication adherence is affected by the individual's various factors and it may be necessary to adopt a qualitative approach tailored to individual traits to identify the contextual factors related to medication adherence [25].
The relationships between health literacy, self-efficacy, and medication adherence and the effect of these two variables on medication adherence were identified. The results showed that health literacy did not show a correlation with self-efficacy and medication adherence. This was in contrast with previous research [10]. In addition, health literacy was not shown to influence medication adherence on the regression analysis. It is generally expected that as patients with higher health literacy have greater information regarding medication, they will have greater medication adherence [26]. However, contrary to expectation, previous research showed that higher levels of health literacy resulted in lower levels of medication adherence [26]. This is because medication adherence is a complex phenomenon affected by multiple factors [27]. Thus, health literacy alone is not sufficient in explaining medication adherence. This is most likely due to the fact that older people with chronic illnesses understand the circumstances that require them to take their medications and view it as a natural part of their life [28]. Additionally, during the data collection process, many participants in this study revealed that they did not wish to burden their families with their diseases. Because of this reason, medication intake in older people may be more greatly influenced by psychological reasons than by health literacy itself.
Self-efficacy was shown to be a factor influencing medication adherence in the older people with polypharmacy. This was similar to previous research that studied older people with chronic illnesses [11]. Older people with polypharmacy consume a large number of drugs for extended periods because they are vulnerable to diseases due to aging. However, a reduction in cognitive ability and the complexities of drug intake caused by polypharmacy may make it difficult for these people to adhere to their regimen properly [25]. In nursing, self-efficacy is a key concept in explaining the maintenance of specific health behaviors such as medication adherence [24]. This is because high self-efficacy enables one to overcome difficulties and successfully change one's behavior. As older people with polypharmacy take their medication for a long duration, successful medication adherence depends more on self-motivation than on the insistence of others. Thus, nurses should actively seek methods to increase self-efficacy. By referring to previous research which has managed to enhance self-efficacy by using interventions with regular reminding [29] and education using images [15], new nursing interventions that employ linguistic arousal, direct experiences, and accomplishments to increase self-efficacy should be applied to older people with polypharmacy. Most previous research that sought to identify the factors influencing medication adherence of older people focused on hypertension or diabetes [6,20]. Thus, this study seeks to build on previous research and ascertain the influences of health literacy and self-efficacy on medication adherence in older people with polypharmacy. However, a drawback of this study is that it has a relatively small sample size compared to previous research. Since previous studies have identified health literacy and self-efficacy as key variables in explaining medication adherence [10,11], it seems necessary to conduct further studies with a larger number of participants.
This study has the following limitations. First, the existing tools for evaluating medication adherence deal exclusively with prescription drugs. Consequently, future research, which aims to be more comprehensive and to evaluate medication adherence with regard to prescription and non-prescription drugs, seems justified. This is because polypharmacy complicates medication intake and may subsequently influences medication adherence [25]. Second, although the number of over-the-counter drugs approved by the Ministry of Drug and Food Safety of Korea is 10,775 [30], this study has constrained the scope to non-prescription drugs, thereby limiting the study. To overcome this problem, this study created a separate open-ended question in the survey that asked about other non-prescription drugs consumed by the participants, but this was not effective, as the response rate was low. Therefore, it is prudent to conduct future research that categorizes over-the-counter drugs more systematically to attain a more accurate picture. Third, technical problems were encountered in this study. The non-prescription drugs included in this survey were classified under relevant Korean laws into two separate categories: over-the-counter drugs and health-functional foods. However, most individuals are incapable of precisely distinguishing between the two [17]. They are in the form of capsules or purified tablets, making their exact classification more difficult. It is likely that the participants in this study were incapable of distinguishing between the two. Therefore, in future studies including non-prescription drugs, subjects should be required to carry their medication so that the surveyor can check the labels and differentiate between over-the-counter drugs and health-functional foods by referring to the website of the Korean Pharmaceutical Association. Finally, as this study took its sample from a single center in Seoul, its general applicability is circumscribed. Therefore, repeated studies with larger sample sizes and more areas are recommended.
CONCLUSION
This study aims to identify the relationship between health literacy, self-efficacy, and medication adherence and the factors that influence medication adherence in order to present basic data required to develop nursing interventions that can enhance medication adherence in older people with polypharmacy. Since it is expected that polypharmacy in older people will increase as society ages and the prevalence of chronic diseases increases, it seems necessary to conduct repeated research in order to identify ways to improve medication adherence.
Notes
Authors' contribution
Study conception and design acquisition - JYC and SJC; Data collection - JYC; Analysis and interpretation of the data - JYC and SJC; Drafting and critical review of the manuscript - JYC and SJC; Final approval - JYC and SJC
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
This article is a revision of the first author's master's thesis from Seoul National University.