The impacts of nurses' attitudes towards dementia, critical reflection competency, and nursing work environment on person-centered nursing in acute care hospitals: A descriptive study
Article information
Abstract
Purpose
The purpose of the study was to examine the attitudes of acute care nurses towards dementia, their critical reflection competency, and the level of nursing work environment and to identify the factors relating to person-centered nursing.
Methods
The study was conducted for 149 nurses with at least 1 year of experience working in acute care hospitals and providing nursing care to hospitalized elderly patients. The measurements used were the Dementia Attitude Scale Korean version, the Critical Reflection Competency Scale, the Nursing Work Environment Scale, and the Person-Centered Nursing Assessment Tool. The collected data were analyzed with frequency analysis, descriptive statistics, independent t-test, ANOVA test, Pearson's correlation, and multiple regression using IBM SPSS 29.0 software.
Results
The factors influencing person-centered nursing performance were critical reflection competency (β=.49, p<.001), attitudes towards dementia (β=.29, p<.001), and clinical career (β=-.26, p=.024), having the explanation power of 59.6%.
Conclusion
The results of this study indicate that critical reflection competency, attitudes towards dementia, and clinical career have an impact on person-centered nursing performance. Specifically, higher levels of critical reflection competency and positive attitudes towards dementia were predictors with higher levels of person-centered nursing performance. Therefore, to enhance person-centered nursing performance among acute care nurses, it is important to prioritize critical reflection training programs for experienced nurses to enhance their critical reflection competency.
INTRODUCTION
1. Significance of the Study
In Korea, the proportion of adults aged 65 years and older of the total population is 17.5% in 2022 [1]. Furthermore, the number of older adults with dementia and the overall older adult population are increasing rapidly. The number of older adults with dementia living in communities receiving hospital care for acute illnesses is increasing, along with the number of nurses caring for older adults with dementia in acute care hospitals [2]. Notably, the ratio of hospitalization days to outpatient visits for older adults with dementia in tertiary and general hospitals has increased annually from 27% in 2008 to 55% in 2017 [3].
The unfamiliar hospital environment during acute care stays can lead to behavioral issues in older adults with dementia. A retrospective cohort study found that 45.8% of patients with dementia in 10,014 hospitals developed delirium during hospitalization. Furthermore, older adults with dementia experience higher mortality, higher incidence of falls, decreased function, and an increased risk of malnutrition, pain, fear, and overstimulation compared to the general population [4]. Person-centered nursing for older adults with dementia focuses on providing individualized services, understanding psychological needs, creating a physical environment that preserves personal "respect" and "dignity," and establishing an autonomous decision-making structure for older adults with dementia [5]. This approach can reduce the behavioral and psychological symptoms of dementia and help maintain and improve cognitive function, making it a critical factor in caring for older adults with dementia [6]. However, acute care hospitals primarily concentrate on treating the disease [2]. Accessing person-centered nursing with standardized protocols within the current healthcare system for older adults with severe, complex, chronic diseases and a wide range in physical, cognitive, and functional abilities among individuals is either impossible or severely limiting [7]. As the demand for specialized nursing care in the aging era increases, the provision of quality care through a comprehensive understanding of the person, in addition to the patient's disease, becomes fundamental to the modern nursing environment [8]. Further, there is a growing demand for nurses to provide care to older adult patients with dementia as a medical condition. Therefore, it is essential to analyze the factors that impact nurses' ability to deliver person-centered nursing care. This analysis encompasses examining attitudes toward dementia as an individual factor and assessing critical reflection competency and the nursing work environment as organizational environmental factors.
At the individual level, positive attitudes toward dementia can aid in focusing on care for individuals with dementia and delivering person-centered nursing [2]. Moreover, attitudes toward dementia were positively correlated with person-centered nursing [9] — suggesting that positive attitudes toward dementia are essential for improving quality of care.
Critical thinking disposition, the ability to gather information from a situation and draw necessary conclusions through reasoning, has been positively correlated with person-centered nursing [10]. Nurses who effectively apply critical reflection develop strategies that promote an individualized, holistic approach to patient care and constantly strive to improve their professional competence [11]. Individuals with high critical reflection competencies actively learn to practice professional nursing. They are rewarded with positive feedback to adapt their practice to the needs of individual patients, which can be an essential factor in providing person-centered nursing care.
At the organizational level, the nursing work environment, which includes sufficient time, organizational support, and a collaborative relationship between the client and the healthcare team, is critical for providing appropriate care [8]. Positive perceptions of the nursing work environment are associated with higher levels of job satisfaction and lower rates of burnout, leading to higher-quality nursing care [12]. In acute care hospitals, where patients with various conditions, frequent emergencies, and high severity are cared for, the work environment, including adequate staffing, resources, and support for individual nurses, may also significantly affect the implementation of person-centered nursing.
Studies have analyzed the factors affecting the performance of person-centered nursing. Nonetheless, these studies are insufficient, and previous studies have reported conflicting results regarding the effects of the nursing work environment on person-centered nursing [13,14]. Additionally, since acute care is provided in general hospitals focusing on "disease," there is a lack of research on nurses caring for older people with dementia as an underlying disease.
Therefore, person-centered nursing is an important concept that should be considered in acute care hospitals where the number of older adults with dementia increases with age. Furthermore, the present study analyzes the obstacles to person-centered nursing and proposes improvements.
2. Research Objectives
This study aimed to identify nurses' attitudes toward dementia, critical reflection competency, and nursing work environment. Furthermore, it sought to identify factors affecting person-centered nursing performance.
The specific objectives were as follows:
1) Identify the general characteristics of participants.
2) Determine participants’ attitudes toward dementia, critical reflection competency, the nursing work environment, and person-centered nursing performance.
3) Identify differences in person-centered nursing performance based on participants' characteristics.
4) Analyze the relationship between attitudes toward dementia, critical reflection competency, nursing work environment, and person-centered nursing performance.
5) Identify factors such as attitudes toward dementia, critical reflection competency, and the nursing work environment influencing person-centered nursing performance.
METHODS
Ethical statement: This study was approved by the Institutional Review Board (IRB) of Samsung Medical Center (IRB No. 2023-02-060, 2023-02-060-001). Informed consent was obtained from the participants.
1. Study Design
This descriptive study used a survey to assess the attitudes of acute care hospital nurses toward dementia, their critical reflection competency, and their perceptions of the nursing work environment. Additionally, it aimed to identify factors that impact person-centered nursing performance.
2. Study Participants
The participants were nurses in acute care hospitals with at least 1 year of experience providing nursing care to inpatients aged 65 and older. The exclusion criterion was nurses working in departments that did not provide direct care to older patients, such as pediatrics or operating rooms.
The number of participants required for the study was calculated using the G power 3.1 and 9.7 programs. Moreover, the multiple regression analysis yielded a moderate effect size of .169 based on the coefficient of determination R²=.14 based on previous studies [15]. Given a significance level of .05, a power of .80, and 18 independent variables (comprising 15 general characteristics and three main independent variables), a minimum sample size of 135 was required. Therefore, this study recruited 149 participants, considering a 10% dropout rate based on previous studies [14]. The data from all 149 participants were used in the final analysis.
3. Research Tools
1) General Characteristics of Participants
The general characteristics included sex, age, marital status, highest level of education, current department, total clinical experience, type of care provided, average number of patients per shift, dementia-related education, presence of a family member with dementia, and living with a family member with dementia.
2) Attitudes Toward Dementia
This study used the Dementia Attitudes Scale Korean version (DAS-K) developed by O'Connor and McFadden [16] and later translated by Chang et al. [17]. The DAS-K comprises 20 questions, divided into a 10-item dementia knowledge scale to assess cognitive attitudes toward dementia and a 10-item social comfort scale to assess emotional and behavioral responses. These questions are further grouped into four subscales: understanding the person with dementia, social discomfort, social comfort, and willingness to provide person-centered nursing. Each item is scored on a seven-point Likert scale, with 1 being "not at all" and 7 being "very much," with six reverse-scored items. The total score ranges from 20 to 140, with higher scores indicating more favorable attitudes toward dementia and older adults with dementia. The Cronbach's α was .83 at the time of tool development [16], .85 for 20 items with .78~.84 for four sub-factors in Chang et al.’s study [17], and .90 in this study.
3) Critical Reflection Competency
Critical reflection competency was measured using the Korean version of the Critical Reflection Competence Measurement Tool developed and translated by Shin et al. [11]. This instrument comprises 19 items, each scored on a five-point Likert scale ranging from 1 (not at all) to 5 (strongly agree). The total score ranges from 19 to 95, with higher scores indicating higher critical reflection competence in the clinical nursing environment—Cronbach's α was .85 at the development [11] and .91 for this study.
4) Nursing Work Environment
The Korean version of the Practice Environment Scale of the Nursing Work Index was developed by Lake [18] and validated by Cho et al. [19]. The instrument comprises 29 questions, including four questions on "sufficient workforce and material support," nine questions on "foundation for quality nursing care," nine questions on "nurses' participation in hospital management," three questions on "nurses' cooperation with doctors," and four questions on "nursing managers' competence, leadership, and support for nurses." Each item was scored on a four-point Likert scale, with 1 being "not at all true" and 4 being "very true." The score is the average of all items and ranges from 1 to 4. The higher the score, the better the nurses’ perceived work environments. Cronbach's α was .82 when Lake [18] developed the instrument and .93 with .80~.84 for each subscale in Cho et al.'s [19] study. In this study, Cronbach's α was .94.
5) Person-Centered Nursing Performance
Person-centered nursing performance was measured using the Lee’s [20] Person-centered Nursing Assessment Tool. The tool comprises 25 questions in five subdomains: four questions on empowerment, four questions on wholeness, five questions on individualization, five questions on respect, and seven questions on relationships. The tool is a five-point Likert scale, with 1 being "not at all" and 5 being "very much." The score is the average of the total scores and ranges from 1 to 5. A higher score indicated a higher level of person-centered nursing performance. The reliability of this tool was Cronbach's ⍺ at .94 with .80~.89 for each factor in Lee's [20] study. In this study, Cronbach's α was .94.
4. Data Collection
Data collection for this study was conducted anonymously through an online survey from March 11, 2023, to April 5, 2023, after receiving approval from the Institutional Review Board (IRB) of Samsung Medical Center. After explaining the study's purpose and data collection methods thoroughly to the nursing department of the affiliated acute care hospital, the researcher received approval for data collection. Subsequently, a notice was distributed to all hospital departments, and those interested in participating accessed the study using QR codes. Also, Participants were recruited through announcements on the "My Duty" bulletin board, an online application used to manage nurses' work, and Naver cafés dedicated to preparing for graduate school admission. A link to the Google Online Questionnaire was shared, and interested individuals were invited to complete a survey. Participation was contingent upon their voluntary agreement after reading the study description, which included information about the study’s purpose, procedures, potential risks and benefits, compensation for losses resulting from participation in the study, voluntary participation, withdrawal of consent, and protection of personal information.
5. Data Analysis
The data collected in this study were analyzed using SPSS version 29.0 (IBM Corp.). The specific methods of analysis are as follows:
1) The participants’ general characteristics were analyzed using frequencies, percentages, means, and standard deviations.
2) Participants' attitudes toward dementia, critical reflection competency, the nursing work environment, and person-centered nursing performance were analyzed using means and standard deviations.
3) Differences in person-centered nursing performance according to general characteristics were analyzed using an independent t-test or ANOVA. Post-hoc tests were performed using Scheffé’s tests.
4) Correlations between attitudes toward dementia, critical reflection competency, and person-centered nursing performance according to the nursing work environment were analyzed using Pearson's correlation.
5) Factors affecting nurses’ person-centered nursing performance in acute care hospitals were analyzed using multiple regression analysis.
6. Ethical Considerations
Before conducting this study, approval was obtained from the IRB of Samsung Medical Center in Seoul, Korea (IRB No. 2023-02-060, 2023-02-060-001). Permission was obtained from the hospital's nursing department before data collection. Participants were provided with sufficient information regarding the purpose and content of the study. Moreover, the questionnaire was administered if the participants voluntarily agreed to participate in the study. Nurses who participated in the study were given a coupon worth 5,000 won as an appreciation token. The survey content was anonymized and used only for research purposes. Personal contacts collected for rewards were permanently deleted immediately after bonuses were provided. All personal information is kept secure, and research-related materials are stored in a separate place with a lock for a mandatory storage period of 3 years. They will be permanently deleted immediately after the storage period.
RESULTS
1. General Characteristics of Participants
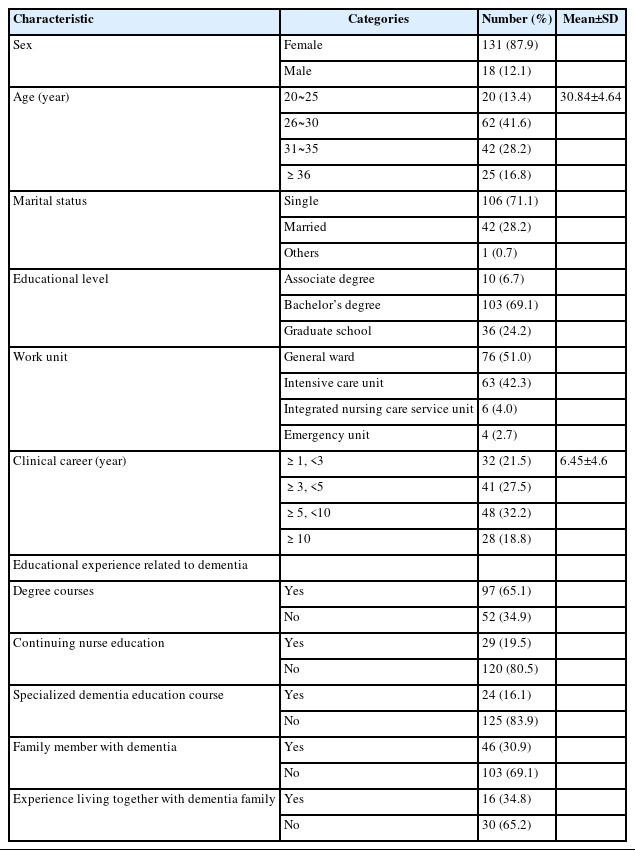
The general characteristics of the study participants are presented in Table 1. The participants included 131 female (87.9%) and 18 male (12.1%), with an average age of 30.84±4.64 years. Most participants were single (n=106, 71.1%) or university graduates (n=103, 69.1%). The participants worked in internal and surgical wards (n=76, 51.0%), intensive care units (n=63, 42.3%), nursing and care integrated service wards (n=6, 4.0%), or emergency departments (n=4, 2.7%), with an average of 6.45±4.60 years of clinical experience. Ninety-seven participants (65.1%) had received dementia education during their degree program, 29 (19.5%) through continuing education, and 24 (16.1%) completed specialized dementia education courses. Regarding having a family member with dementia, 46 participants (30.9%) answered "yes." Of them, 16 (34.8%) lived with a family member with dementia.
2. Participants' Attitudes Toward Dementia, Critical Reflection Competency, Nursing Work Environment, and Person-Centered Nursing Performance
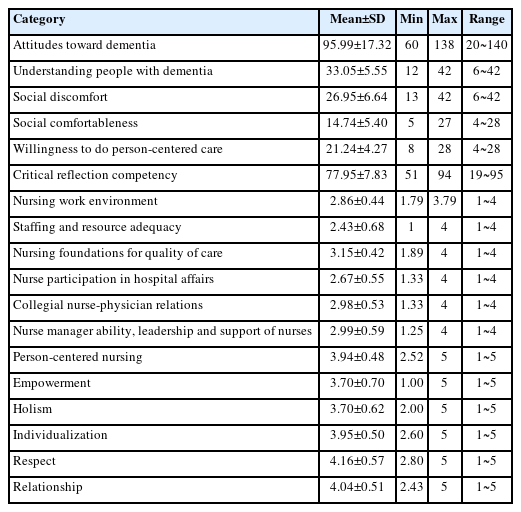
Participants’ attitudes toward dementia, critical reflection competency, nursing work environment, and person-centered nursing performance are shown in Table 2. The score of attitude toward dementia was a mean of 95.99±17.32 out of 140 points. The scores of subdomains were 33.05±5.55 for an understanding of individuals with dementia, 26.95±6.64 for social discomfort, 14.74±5.40 for social comfort, and 21.24±4.27 for willingness to provide person-centered nursing. Critical reflection competency averaged 77.95±7.83 out of 95. The nursing work environment was 2.86±0.44 out of 4, with sub-scores of 2.43±0.68 for sufficient staffing and material support. Further, it was 3.15±0.42 for the foundation for quality nursing care, 2.67±0.55 for nurses' participation in hospital operations, 2.98±0.53 for nurses' collaboration with physicians, and 2.99±0.59 for nursing managers' competence, leadership, and support for nurses. Person-centered nursing had a mean score of 3.94±0.48 out of 5, with subscales of 3.70±0.70 for empowerment, 3.70±0.62 for wholeness, 3.95±0.50 for individualization, 4.16±0.57 for respect, and 4.04±0.51 for relationships.
3. Differences in Person-Centered Nursing Performance by General Characteristics
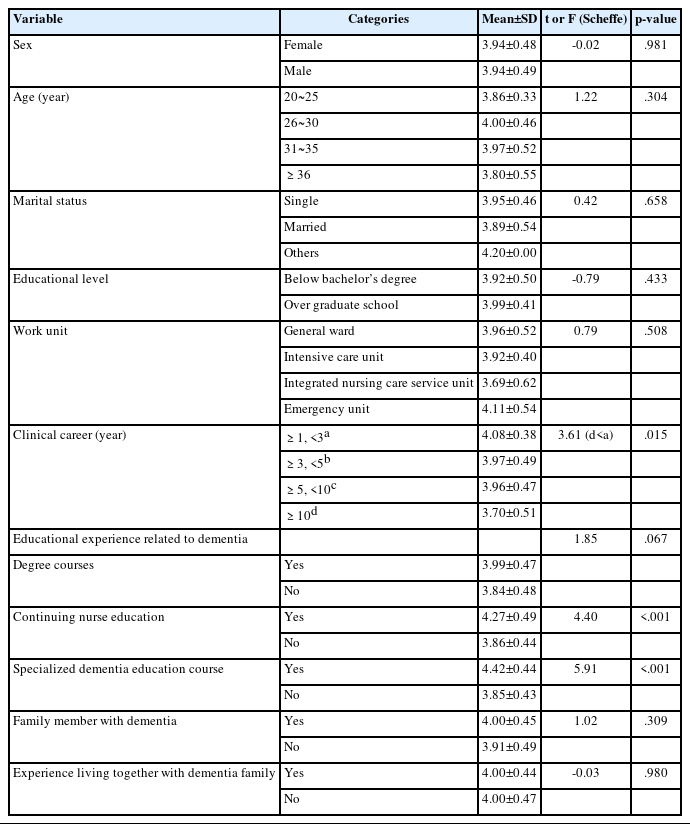
Differences in person-centered nursing performance according to general characteristics are shown in Table 3. There were significant differences in person-centered nursing performance according to clinical experience (F=3.61, p=.015), continuing education (t=4.40, p<.001), and dementia specialty training (t=5.91, p<.001). Scheffe's post-hoc test for clinical experience showed that those with less than 1~3 years of experience had a higher level of person-centered nursing performance than those with more than 10 years of experience. Additionally, those who completed dementia-related continuing education and specialized dementia education courses had a higher level of person-centered nursing performance than those who had not.
4. Correlations Between Attitudes Toward Dementia, Critical Reflection Competency and Nursing Work Environment, and Person-Centered Nursing Performance
Correlations between attitudes toward dementia, critical reflection competency, nursing work environment, and person-centered nursing are shown in Table 4. Person-centered nursing performance was significantly and positively correlated with attitudes toward dementia (r=.669, p<.001), critical reflection competency (r=.704, p<.001), and nursing work environment (r=.443, p<.001). Specifically, the more positive the attitude toward dementia, the higher the critical reflection competency. And the better the nurses’ perceived nursing work environment, the higher their level of person-centered nursing.
5. Factors Affecting the Person-Centered Nursing Performance
Factors affecting person-centered nursing performance are shown in Table 5. We analyzed the factors affecting person-centered nursing performance by selecting age, clinical career, educational experience related to dementia in continuing nursing education, educational experience related to dementia-specialized dementia education courses, attitude toward dementia, critical reflection competency, and the nursing work environment as independent variables for multiple regression analysis. Dummy variables included whether or not the nurse had completed continuing education on dementia and whether or not the nurse had completed a specialized training course on dementia. The minimum value of the regression standardized residual was -2.76, and the maximum value was 2.54. The standardized deviation was 0.98, and normality was confirmed using P-P diagrams and histograms. The tolerance limits were 0.21~0.70, more than 0.1, and the Variance Inflation Factor values were 1.44~4.82, which were not greater than 10, indicating no risk of multicollinearity.
Regression analysis showed that among the variables, critical reflection competency (β=.49, p<.001), attitude toward dementia (β=.29, p<.001), and clinical experience (β=-.26, p=.024) were influential factors. The explanatory power was 59.6% (F=32.18, p<.001). Specifically, the higher the clinical experience, the lower the person-centered nursing performance. Additionally, the higher the critical reflection competency or the more positive the attitude toward dementia, the higher the person-centered nursing performance.
DISCUSSION
By analyzing the factors influencing person-centered nursing in acute care hospitals, this study provides a rationale for developing strategies to improve person-centered nursing. The score of person-centered nursing in this study was 3.94±0.48 out of 5. This is relatively low among the empowerment and wholeness subdomains. This study focused on shift nurses providing direct care, consistent with a study that found that shift nurses providing direct care had lower levels of perceived structural empowerment than permanent or outpatient nurses [21]. Previous studies have shown that an essential factor in providing person-centered nursing is environmental support that can provide immediate help from professional personnel at the right time [22]. Thus, general hospitals still experience a vicious cycle of staff shortages and work environments [23].
The factors affecting person-centered nursing performance in this study were critical reflection competency, attitude toward dementia, and clinical career. Among these factors, critical reflection competency was the most crucial in improving person-centered nursing performance, confirming the importance of strengthening critical reflection competency for nurses. It is necessary to provide nurses with opportunities to reflect on their nursing practice and discover the meaning of nursing through a critical reflection training program that comprises the process of understanding the concept of critical reflection, strengthening its strategies, and applying them to enhance critical reflection competency [24]. Moreover, the exchange of opinions and reflections based on clinical cases should be encouraged in clinical settings. Additionally, as there is a lack of research on the relationship between critical reflection competency and person-centered nursing performance in clinical nurses, studies that apply critical reflection training programs in practice are needed. The second factor affecting person-centered nursing performance was nurses’ attitudes toward dementia. This is similar to previous studies [9] that found that nurses’ attitudes toward dementia were significantly associated with person-centered nursing. Nurses’ attitudes toward dementia are considerably better when they receive dementia-related education [2]. Notably, nurses in nursing homes with a high proportion of dementia patients have positive attitudes toward older adults with dementia [25]. Thus, dementia-related education is important for fostering positive attitudes toward dementia among nurses in acute care hospitals.
Among the general characteristics in this study, clinical career negatively affected person-centered nursing performance, similar to the results of a previous study [26] that showed that the lower the total clinical career, the higher the degree of person-centered nursing. Nurses with more experience experienced higher job stress [27]. A previous study of nursing home nurses [28] showed that job stress was negatively related to person-centered care. Therefore, applying the Stress Management and Resiliency Training (SMART) program to experienced nurses is expected to reduce stress, improve resilience [29], and increase person-centered nursing performance.
Conversely, in this study, the nursing work environment did not significantly influence person-centered nursing, which is consistent with the findings of Kang and Seo [13]. Although there was a positive correlation between the two variables, nurse burnout and psychological stress caused by a negative work environment were expected to be more critical variables in person-centered nursing than the nursing work environment itself. Previous studies have shown that nurses' burnout increases when their work environment is poor [8] and that burnout significantly affects person-centered nursing [14]. Therefore, future studies are needed to compare the perceived nursing work environment according to hospital size, department, and average number of patients per capita. This includes considering nurses' burnout and psychological stress and verifying their relationship with person-centered nursing performance.
As the population ages, older adults with dementia are often admitted to acute care hospitals for treatment. Hence, acute care nurses should provide person-centered nursing to older adults with dementia. Acute care hospital nurses need to perform person-centered nursing without experiencing psychological burdens when caring for older patients with dementia. Thus, acute care hospitals must offer critical reflection training programs and dementia-related educational opportunities to experienced nurses with relatively low levels of person-centered nursing performance. This should be extended to nurses throughout the hospital to improve individual competencies and lay the foundation for providing person-centered nursing for older adults with dementia in acute care hospitals.
CONCLUSION
This study aimed to investigate the impact of attitudes toward dementia, critical reflection competency, and the nursing work environment on person-centered nursing performance among nurses in acute care hospitals. The goal was to improve the quality of care for older adults, given the increasing hospitalization of older adults with dementia due to an aging society. The findings identified critical reflection competency, attitudes toward dementia, and clinical experience as factors affecting person-centered nursing. Therefore, to improve person-centered nursing performance, it is necessary to implement critical reflection training programs to strengthen nurses’ critical reflection competency and expand opportunities for nurses to regularly complete dementia-related educational programs to understand and perceive older adults with dementia positively. Furthermore, clinical nursing guidelines for caring for older adults with dementia are required to reduce nurses’ psychological burden and lay the foundation for improving the performance of person-centered nursing.
The significance of this study is that it provides a basis for developing strategies to improve person-centered nursing among nurses in acute care hospitals. This study collected comprehensive data from nurses with experience in caring for older adult patients to analyze the general factors affecting the performance of person-centered nursing for older adults with dementia. However, the person-centered nursing tool used in this study was not developed specifically to care for older adults. Thus, the questions themselves had limitations in reflecting the uniqueness of older patients. Therefore, based on the main findings and limitations, we make the following suggestions: First, it was necessary to verify the effectiveness of the proposed critical reflection training. In particular, this should be applied to nurses' careers and analysis of their person-centered nursing performance before and after training. Second, it is necessary to develop a person-centered nursing scale that considers older adults’ characteristics. Third, we recommend a follow-up study involving nurses with expertise in caring for older adults with dementia.
Notes
Authors' contribution
Study conception and design acquisition - MK and SS; Data collection - MK; Analysis and interpretation of the data - MK and SS; Drafting and critical revision of the manuscript - MK and SS
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
This article is a revised version of the first author’s thesis.