Living experiences of older patients with cancer amid the COVID-19 pandemic: A phenomenological study
Article information
Abstract
Purpose
Patients with cancer experience psychological and social problems; in particular, older patients with cancer face many difficulties during the cancer treatment process owing to aging and underlying diseases. Furthermore, the lives of individuals may be impacted by the COVID-19 pandemic. Therefore, the purpose of this study is to describe the experiences of older patients with cancer during the cancer diagnosis and treatment process amid the COVID-19 pandemic.
Methods
This study employed a qualitative, descriptive phenomenological approach to explore and analyze the experiences of the participants. The participants in this study consisted of patients aged over 65 who were diagnosed with cancer, and data were collected from May 4 to June 30, 2022 through in-depth individual interviews. The collected data were analyzed using Giorgi’s phenomenological analysis.
Results
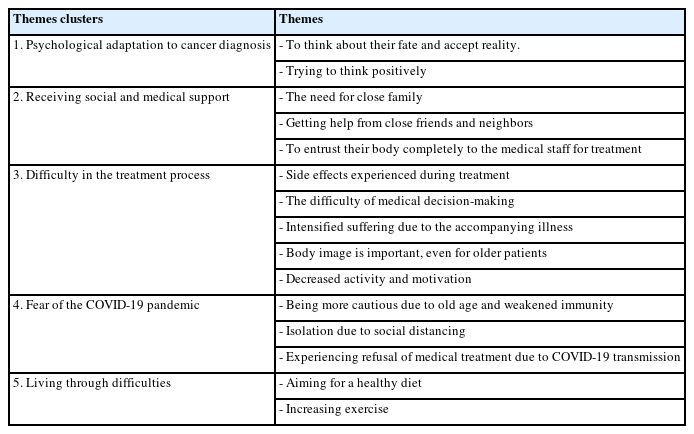
Participants were six older patients with cancer with an average age of 69.66 years. Five theme clusters and 15 themes were generated. The theme clusters were “psychological adaptation to cancer diagnosis,” “receiving social and medical support,” “difficulty in the treatment process,” “fear of the COVID-19 pandemic,” and “living through difficulties.”
Conclusion
This study revealed that older patients with cancer demonstrated a unique psychology about how to accept the shock of the diagnosis and the resulting coping patterns and feelings of depression. Additionally, it was verified that older patients with cancer, susceptible to infections due to their advanced age and weakened immunity, also face an increased vulnerability to COVID-19. Therefore, a support system tailored to the characteristics of older patients with cancer should be established.
INTRODUCTION
1. Background
The World Health Organization (WHO) predicts that between 2015 and 2050, the proportion of the world’s population aged over 60 will increase from 12% to 22% [1]. Korea has one of the fastest-aging populations in the world [2]. According to national cancer registration statistics, one in 25 people (3.9% of the country’s total population) are currently undergoing cancer treatment or are survivors of cancer [3]. The cancer survival rate is rising due to recent developments in medical technology. Among all cancer patients, patients with cancer aged 65 or older account for 46.4%, and this proportion is gradually increasing [3,4]. Moreover, the older adult population in Korea accounted for 12.8% of the total population in 2015 and will expand to 20.3% in 2025; the proportion of older patients with cancer is also expected to increase as Korea becomes a super-aged society [5].
Patients with cancer undergo multiple stages of psychosocial experiences, including acute and transitional survival stages, extended survival stages, and chronic or permanent survival; simultaneously, they not only experience diagnosis, staging, actual treatment-related emotions, recurrence, financial problems, and psychosocial sequela, but they also have requirements that vary depending on age and the accompanying disease [6,7]. Hence, to meet the needs of older cancer survivors and improve their quality of life (QoL), older patients with cancer should receive deeper attention [7,8].
In older patients with cancer, risk factors include comorbidities, multiple drug administration, cognitive decline, and decreased physical function, which, unlike younger patients, may introduce additional complexities in cancer treatment with potential risks [9]. In particular, older patients with cancer experience a higher degree of functional decline than older patients with other chronic ailments; moreover, young patients with cancer perceive cancer as a hurdle to be overcome and actively treated, whereas older patients with cancer perceive the disease as leading to death. Older patients with cancer have a low willingness to pursue active treatment; they may wish to live the rest of their lives comfortably and without pain rather than undergo treatment [10]. Additionally, they experience loss due to bereavement from their spouse or close friends passing away, as well as a reduced social role and economic burden owing to retirement [11].
As such, older patients with cancer may experience difficulties in their lives, including physical, emotional, and economic problems, along with social isolation due to the burden of not only the aging process but also cancer treatment. In addition, older patients with cancer are classified as a more high-risk group than any other group in the COVID-19 pandemic context [12]. The total number of confirmed COVID-19 cases nationwide from the initial outbreak until March 10, 2020 was 7,513; notably, 5,663 of these cases were concentrated in a specific region. The average age at the time of death was 75.5 years, and the older adult population showed a higher fatality rate compared to other age groups [13]. This national disaster can affect the cognition and psychology of older patients with cancer classified as high-risk individuals for infection, potentially exacerbating their suffering.
In this study, in-depth interviews were held with older patients with cancer to understand their circumstances and experiences during cancer diagnosis and treatment. The objective of this study is to delve into the rationale for nursing interventions tailored to older patients with cancer, encompassing physical, psychological, and social interventions. Additionally, it seeks to identify the vulnerability of older patients with cancer as recipients of treatment during the COVID-19 pandemic and elucidate the necessity for support. Giorgi’s phenomenological approach was adopted to identify the meaning of the situations and experiences during the treatment process of older patients with cancer and to use the findings as basic data for developing efficient, individual nursing interventions based on patients’ needs [14]. Phenomenology involves exploring and integrating what individuals have experienced and how they have experienced it. Giorgi’s phenomenology necessitates a return to specific lived situations [14]. Therefore, adopting Giorgi’s phenomenology in this study is expected to be beneficial for developing suitable interventions based on the specific experiences of older adults with cancer.
2. Study Purpose
The purpose of this study was to deeply understand their experiences and situations during cancer diagnosis and treatment amid the COVID-19 pandemic.
METHODS
Ethic statement: This study was approved by the Institutional Review Board (IRB) of Keimyung University (IRB No. 40525-202203-HR-010-02). Informed consent was obtained from the participants.
1. Study Design
This study employed a qualitative, descriptive phenomenological approach involving in-depth personal interviews to gain a comprehensive understanding of the experiences of patients aged 65 or older during cancer diagnosis and treatment. The overall process of the study was written by following the consolidated criteria for reporting qualitative research (COREQ) guidelines [15].
2. Participants
Participants were older patients aged 65 or above who were diagnosed with cancer and undergoing treatment such as surgery, chemotherapy, or radiation therapy, or those who were being followed up with after treatment. The participants were six patients who visited a tertiary general hospital as outpatients for cancer treatment, and after hearing an explanation of this study, they expressed their intention to participate. Exclusion criteria included those who had difficulties with communication due to hearing or vision impairments or other physical ailments, had difficulty in consenting based on not sufficiently understanding the study’s purpose due to mental illness or dementia, and were in hospice palliative care while receiving treatment or for whom a life-sustaining medical plan had been created.
3. Data Collection
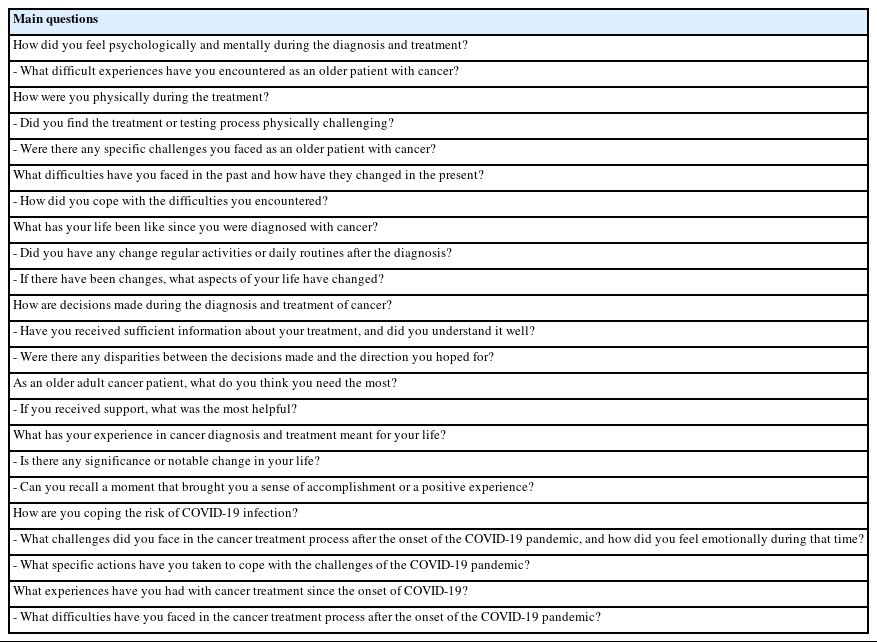
We collected data from May 4 to June 30, 2022. The meeting room in the hospital that the participants visited was used to gather the data. We used a ‘criterion sampling’ method for participant recruitment, targeting older patients aged 65 and above who were diagnosed with cancer and undergoing treatment. In-depth interviews were held once or twice with each person, and each interview lasted approximately 43 to 86 minutes. The interview questions were constructed with collaborators based on references after the researcher selected a topic (Table 1). The collaborators have experience conducting qualitative and mixed-methods research, with published papers in international academic journals and domestic accredited journals. Additionally, the collaborators participated in the analysis, categorization, and validation of interview content. Each interview was transcribed and checked to see if repeated content or new perspectives appeared, and the interviews were stopped when the data were judged to be sufficiently saturated.
4. Data Analysis
Phenomenological suspension of judgment requires returning to a state of open exploration, free from any preconceptions or biases. The researchers aimed to recognize and set aside preconceived notions when studying older adults with cancer. Examples of preconceptions include “treatment motivation in older adults with cancer,” “desire for a return to normalcy,” and patients’ expectations that various challenges, including physical, social, economic, and psychological hardships, would emerge even after surviving cancer.
This study was conducted to uncover the experiences of older adults with cancer and to understand and analyze them from a nursing perspective. Giorgi’s phenomenological research method was used to explore the participants’ experiences of cancer diagnosis and treatment without causal explanation or negative prejudice [14]. First, the researcher transcribed the content of the participants’ experiences verbatim and then repeatedly read the transcripts to grasp the overall outline. Second, using the transcription and field notes, meaningful content was underlined to create a list of semantic units. Third, after discussing the derived meaningful statements with a collaborator, they were expressed in the form of nursing or plain language. Throughout this process, we opted to use nursing and medical terminology, as well as laymen terms, rather than directly quoting the participants’ words. Fourth, the re-expressed meanings were derived by themes and theme clusters. Fifth, the derived results were based on the experiences of older patients with cancer [14,16].
5. Trustworthiness
This study evaluated four factors—credibility, transferability, dependability, and confirmability—according to the qualitative research evaluation criteria presented by Lincoln and Guba [17]. To ensure credibility during the data collection, participants were encouraged to state their thoughts as freely as possible without artificially inducing their statements. In the transcription process, the terms used by the subject were described verbatim, and if a statement required further explanation, the researcher called the participant to check whether the statement was consistent with the stated content instead of arbitrarily describing it. To ensure transferability, meaningful topics were derived through practical experiences by citing the participants’ statements. To ensure dependability and confirmability, meaningful content was derived by reading the transcript independently of the collaborator, and the processes of recording, coding, and categorizing the interview data were presented. The interview data are available to the reader for verification.
6. Ethical Consideration
Prior to the start of the study, approval was obtained from the Keimyung University Institutional Review Board (IRB) (IRB no. 40525-202203-HR-010-02). It was conducted after obtaining permission from the head of the nursing team of the department and the attending physician. Before the interview, the participants were informed about the purpose of the study, confidentiality of the interview content, voluntarily stopping the participation and guarantee of anonymity. During the interviews, the participants’ names and the transcribed content were distinguished only by participant number. After the interviews, a small gift was given to the participants.
RESULTS
Regarding the participants’ general characteristics, there were two male and four female participants, with an average age of 69.7 years; of these, four were married, and two were widowed. Two people were living alone and four were living with their families. Regarding cancer-related characteristics, the participants had been diagnosed with lung cancer (one patient), breast cancer (three patients), liver cancer (one patient), and blood cancer (one patient). The average period of diagnosis was 5.25 years (2.4~8 years). For the diagnosis stage, two patients were in stage 1, one was in stage 2, and three were in stage 4. There were four cases of recurrence or metastasis. Only chemotherapy was performed in three cases, and for surgery, partial resection was performed in one case, and three types of treatment (surgery, chemotherapy, and radiation therapy) were performed in two cases. The average number of chemotherapy and radiation treatments was 23.00 times (4~55 times), and there were three cases of comorbidities including diabetes, hepatitis B, and delirium (Table 2).
Through the integration of meaningful and similar content derived from interviews with these participants, the diagnosis and treatment experiences of older patients with cancer included: “psychological adaptation to cancer diagnosis,” “receiving social and medical support,” “difficulty in the treatment process,” “fear of the COVID-19 pandemic,” and “living through difficulties” (Table 3).
1. Psychological Adaptation to Cancer Diagnosis
Participants were completely unaware that they could be diagnosed with cancer and were shocked by their sudden diagnosis. However, they did their best as parents and thought that the process of death was destiny, and they had the heart to live with a positive mindset and treat life and death equally for their remaining lives.
1) To Think About Their Fate and Accept Reality
Participant 2 contemplated the uncertainty of fate and accepted it as an inherent aspect of life, recognizing that no one can predict the future, and mortality is a universal experience.
“No one knows what I will be like tomorrow after living today.... Everyone dies. Because I have a set life span, I live my life like this, and when my fate comes to me, I have to accept it.” (Participant 2)
2) Trying to Think Positively
Participant 1 experienced enhanced strength and decreased physical discomfort through positive thinking. Participant 2 believed that positive thoughts led to a positive body response.
“When I think, ‘My body isn’t in good state’, it feels like my body hurts more. But when I think, ‘I’m okay, I can fight and win’, it gives me more strength.” (Participant 1)
“When my thoughts turn positive, my body seems to follow to some extent... I even sing songs and play musical instruments.” (Participant 2)
2. Receiving Social and Medical Support
The participants were overcoming the difficulties of the cancer treatment process by relying on close spouses, friends, and medical staff.
1) The Need for Close Family
Participant 1 reported experiencing anxiety and physical discomfort when alone, often worrying about the possibility of dying without anyone knowing, particularly when not with their family.
“Being alone sometimes makes me feel a bit anxious. There are moments when I think, ‘What if I suddenly die one day and nobody knows?’ When I’m with my family at home, I feel better, but being alone makes me feel unwell physically, and it affects my overall condition. It makes me think, ‘I might die alone like this’, and that thought crosses my mind.” (Participant 1)
2) Getting Help From Close Friends and Neighbors
Participant 1 found it challenging to ask her son for help owing to the distance and his own daily routine; therefore, she relied on her friends for assistance for tasks such as going to the hospital.
“My son is far away, and so it is difficult to ask him for help. He also has his own daily routine, and I did not want to interfere with it. My friends around me are the best. It is convenient to ask them for help. ‘Hey, I have to go to the hospital that day. Let’s go together.’” (Participant 1)
3) To Entrust Their Body Completely to the Medical Staff for Treatment
Participant 5 acknowledged their limited knowledge about targeted therapy and medical treatments, emphasizing the importance of trust in the doctor’s expertise and guidance.
“Ordinary people like us do not know well about targeted therapy or what kind of treatment is good, because I am not a person with complete knowledge. We have to trust the doctor because the doctor is speaking to us with knowledge and experience.” (Participant 5)
3. Difficulty in the Treatment Process
The participants experienced considerable pain during the treatment process.
Side effects are experienced not only at the time of surgery or chemotherapy but also afterward. Furthermore, the changes in the body caused by aging and accompanying disease exacerbate side effects. Eventually, after the acute phase, the body and mind become exhausted.
1) Side Effects Experienced During Treatment
Participant 4 experienced unusual sensations in her feet and loose teeth during chemotherapy.
“The most difficult thing is… the soles of my feet seem to have chopped glass and walk on it. I couldn’t walk, that was difficult… and my teeth fell out so I had to apply new dentures.” (Participant 4)
2) The Difficulty of Medical Decision-Making
Participant 2 highlighted that in busy hospitals, medical staff often lack the time to address questions from patients. Participant 5 followed the doctor’s recommendations for her lung cancer treatment because of a lack of information and inability to explore other options or seek advice from others.
“In big city hospitals, there is not enough time to ask questions due to the busy schedule of the medical staff.” (Participant 2)
“I didn’t have much information, so I just followed what the doctor said. I might have wondered about other options or treatments for my lung cancer, but I couldn’t even ask others for advice. So, I just followed the doctor’s recommendations.” (Participant 5)
3) Intensified Suffering Due to the Accompanying Illness
Participant 3 expressed that she experienced discomfort in her legs not only due to the side effects of chemotherapy but also due to stiffening of the joints as a result of aging. Participant 6 shared his medical journey, which began with a fall and led to a diagnosis of cerebral infarction. Subsequent tests revealed an unexpected condition, which doctors identified as leukemia.
“After undergoing chemotherapy, I have a sensation in my soles that feels like someone else’s…. Moreover, my joints and such aren’t in great shape, there are times when they get stiff and all….” (Participant 3)
“After falling down, I became suspicious of something being wrong with my head, so I went to the neurology department, and it was diagnosed as a cerebral infarction…. During various tests, they found strange things, and the doctors said it’s a type of leukemia….” (Participant 6)
4) Body Image Is Important, Even for Older Patients
Participant 4 expressed that losing her hair, especially at the start of chemotherapy, was particularly distressing. She emphasized the importance of appearance, even as a grandmother.
“The worst thing for me was my hair. At the beginning of chemotherapy, I was shocked because my hair and eyebrows fell out. Although I am a grandmother, my appearance is still important.” (Participant 4)
5) Decreased Activity and Motivation
Participant 5 stated that she had lost interest in everything. She felt that her desires had disappeared, possibly because of her age.
“I have lost interest in everything. So sometimes, I even think, ‘Have I ever had depression?’ I used to have such desires. But now, none of that exists. Maybe it’s because of my age.” (Participant 5)
4. Fear of the COVID-19 Pandemic
Participants were afraid due to the fear of infection. They knew that they were in a high-risk group due to older age, had low immunity and underlying diseases, and were trying to strictly follow basic precautions. However, in some cases, participants experienced instances where they were denied medical treatment.
1) Being More Cautious Due to Old Age and Weakened Immunity
Participant 1 reported that a relative of hers, who was in poor health, died from a COVID-19 infection. Having observed this, and being aware of her own weak immune system, she was worried about getting infected.
“My relative, who wasn’t in good health, passed away due to a COVID-19 infection. Having witnessed such a situation and considering that I have a weak immune system, I often think that I shouldn’t get infected.” (Participant 1)
2) Isolation Due to Social Distancing
Participant 4 mentioned that during the COVID-19 pandemic, she was cautious about not going to crowded places and avoided gatherings.
“During the COVID-19 period, I made sure not to go to crowded places and avoided gatherings when they were strongly discouraged. I refrained from attending social gatherings and took extra precautions as a patient.” (Participant 4)
3) Experiencing Refusal of Medical Treatment Due to COVID-19 Transmission
Participant 6 described a situation where he was en route to the hospital but received a phone call instructing him not to come in. This led to the postponement of his positron emission tomography (PET) scan, and the following week, he was unable to go to the hospital.
“I was on my way to the hospital; I received a phone call telling me not to come in. So, I had to turn back. After that, my PET scan was postponed, and the following week, when I needed to collect my prescription, I couldn’t go to the hospital.” (Participant 6)
5. Living Through Difficulties
After their cancer diagnosis, the participants improved their eating habits and increased their amount of exercise to manage their cancer while also trying to live a dignified life. They also changed their diet to a healthy one containing protein, vegetables, and fruits, and participated in light exercise and walking.
1) Aiming for a Healthy Diet
Participant 4 shared her dietary regime, which included specific amounts of fruit, carbohydrates in the morning, meat at each meal, and eggs. She mentioned that, because of her age, she could not taste these foods properly.
“Eat a certain amount of fruit, eat a certain amount of carbohydrates in the morning, eat a certain amount of meat at each meal, eat eggs, and eat fruit, but they don’t taste good because of my age.” (Participant 4)
2) Increasing Exercise
Participant 1 emphasized the importance of regular exercise and gradual progress.
“Exercising regularly… and exercising every day. At first, I could not walk for 10 minutes. However, because it was repeated step-by-step, currently, I can exercise from 1 hour to 1 hour 30 minutes per day.” (Participant 1)
During the COVID-19 pandemic, older patients with cancer experienced various challenges, including psychological adaptation to their cancer diagnosis, seeking social and medical support, coping with treatment-related difficulties, and dealing with COVID-19-related fears. Older patients with cancer made efforts to adapt to their cancer diagnosis during the pandemic, involving accepting their reality and attempting to empty their minds to lead a more positive life. However, the fear of loneliness had a negative impact on this adaptation process, emphasizing the importance of maintaining relationships, especially with close friends and neighbors. Trusting their medical team and entrusting their bodies entirely for treatment was also observed.
The treatment process posed multiple challenges, including side effects, difficulties in medical decision-making, and increased suffering due to coexisting illnesses. The importance of body image became apparent even for older patients, and a decline in physical activity and motivation was noted, suggesting the need for support in these areas.
Additionally, older adults with cancer exhibited increased caution during the COVID-19 pandemic owing to their age and weakened immunity. Social distancing measures led to feelings of isolation, and some patients faced challenges accessing medical treatment due to COVID-19 concerns, further exacerbating the difficulties in their cancer treatment journey.
Nevertheless, patients made efforts to overcome this challenging period by focusing on maintaining a healthy diet and increasing physical activity. They displayed resilience, strong determination, and hope in facing these difficulties.
DISCUSSION
In this study, Giorgi’s phenomenological method was used to understand and comprehensively analyze the experiences of diagnosis and treatment of cancer in older patients. It was found that a treatment and educational intervention program suitable for the characteristics of older patients with cancer is needed, and studies should be conducted on controlling factors that could affect QoL during the course of treatment.
Cancer diagnosis is accompanied by various emotions, such as uncertainty and hopelessness, which cause psychological pain and lead patients with cancer to develop new identities [10]. Although the participants were shocked to receive a cancer diagnosis in an unexpected circumstance, they had already lived most of their lives and accepted this situation as their fate. They also experienced the need to shift toward positive thinking to actively engage in the treatment process. These results are similar to those of previous studies [10,18]. In other words, both young and older patients require psychological adaptation to cope with cancer. Both groups receive various types of treatment and experience the pain associated with treatment. However, previous studies indicated that older adults primarily used resignation as a psychological adaptation [18]. In contrast, participants in this study demonstrated multifaceted approaches to adaptation, including resignation, maintaining hope, and actively engaging in treatment. Furthermore, owing to the high frequency of complications and differences in viewpoints on life expectancy, older patients with cancer tend to be provided relatively passive treatment compared with younger patients [19].
Moreover, depression, one of the psychological issues experienced by older patients with cancer, is difficult for them to perceive on their own and is often considered a natural phenomenon due to aging, making it difficult to intervene appropriately [20]. Furthermore, depression negatively impacts the effectiveness of cancer treatment and patients’ QoL and older patients express depression differently from younger patients and may appear to show a loss of interest [21]. Therefore, in-depth research is necessary to determine the psychological characteristics of older patients with cancer and to facilitate their decision-making regarding active treatment options by providing interventions to improve QoL and reduce the side effects of cancer treatment.
Social support for patients with cancer is multifaceted and includes instrumental support (e.g., physical/medical support), material support (e.g., financial support), informational support (e.g., advice, education), and emotional support (e.g., empathy) [22]. However, in previous studies, it was suggested that young patients require more social resources [18]. In contrast, this study revealed that older patients with cancer also require the support of family or social resources. The factors supporting the participants in this study included not only medical treatment but also their spouses and close neighbors. This finding was similar to that of a past study on the experience of recovering a sense of ego integrity in older patients with cancer [6].
However, the proportion of older adults living alone in Korea increased from 16.0% in 2000 to 19.8% in 2020 [23], and spousal death and social isolation make older patients vulnerable to not receiving appropriate health care [6]. In a situation where the prevalence of cancer in older adults is rising due to aging [24], social and institutional improvements are needed to compensate for this.
Moreover, the participants were highly dependent on medical staff for treatment decisions. This observation is similar to the experiences of decision-making in older patients with cancer in a study by Kim and Hong [25]. The support provided by medical staff in this situation helps improve QoL by reducing uncertainty and depression [22]. Thus, healthcare professionals need to thoroughly comprehend the physical and psychological characteristics of older patients with cancer and strive to provide optimal treatment to enhance their QoL.
In our study, participants predominantly reported experiencing fatigue and leg numbness as adverse effects of cancer treatment. Additionally, they faced the obstacles of a reduced appetite due to aging and treatment-related side effects. Physical activity and the quality of one’s diet are important factors in improving the prognosis and QoL of patients with cancer. However, owing to side effects related to cancer or its treatment and diseases that accompany aging, the degree of function varies from person to person, making it necessary to consider the best approach [26].
Previous studies have confirmed the benefits of reducing cancer-related burden and improving fatigue through nutritional and exercise interventions suitable for individuals [26,27]. Hence, the condition of older patients with cancer should be evaluated in advance, and an intervention should be applied according to observations of their fatigue, ability to exercise, and food preferences.
The participants in this study consisted of older patients undergoing cancer treatment or follow-up care during the ongoing COVID-19 pandemic. They expressed a profound fear of infection due to their awareness of being high-risk individuals with weakened immunity and underlying health conditions. This finding was similar to the perception of risk and psychosocial responses (such as anxiety and depression) in a study carried out on patients with lung cancer during the COVID-19 pandemic by Hyland and Jim [28]. Older patients with cancer, despite requiring support from their surroundings, encountered challenges such as the loss of a spouse, distant family members, or social isolation. Also, social distancing and staying at home due to the pandemic cause older adults to spend considerable time alone, heightening their feelings of isolation and loneliness [29]. Therefore, during an infectious disease outbreak, special attention is needed for emotional support for older adults with cancer. Solutions can be provided by utilizing remote communication and digital platforms to maintain contact with family and the local community. Moreover, these platforms can be used to provide medical information and offer services such as remote counseling.
Korea’s epidemic prevention system, including social distancing measures, has set a good precedent in mitigating the damage caused by infectious diseases. However, a significant finding from the present study was the occurrence of healthcare gaps for high-risk patients. Notably, some participants from an area experiencing the first outbreak of a mass infection in Korea were denied medical treatment at hospitals where they had previously received follow-up care. In previous studies, cases of medical refusal or delays in treatment for COVID-19 patients were commonly reported phenomena [30].
The potentially fatal consequences of the stigma surrounding new infectious diseases for patients with cancer requiring close monitoring are concerning. This study underscores the need for proactive measures and bridging medical gaps to protect vulnerable groups amidst limited information on new infectious diseases. Hence, it is necessary to prepare for potential risks in future epidemics and establish an improved healthcare system with treatment protocols tailored to the Korean context. In particular, it is imperative to develop and implement a support system that considers the unique characteristics of older patients with cancer.
1. Limitations
In this study, convenience sampling was not performed in the process of selecting participants, but the small sample size also warrants caution when interpreting the results. Additionally, the participants had good functional status in their daily life; thus, it is highly likely that their characteristics influenced the findings. Furthermore, as we explored the overall experience of older patients with cancer, since many common themes emerged, there may be limitations in uncovering significant meanings specific to certain situations. Nonetheless, the participants exhibited a positive and hopeful attitude regardless of the stage of their cancer or not having been cured yet. This study has unveiled meanings, including perspectives on older patients with cancer that diverge from conventional knowledge, offering valuable insights. It has also highlighted the necessity for support to groups that may be vulnerable during situations such as infectious diseases and other disasters. In future studies, it will be necessary to consider the various cancer stages and functional states of older patients with cancer.
CONCLUSION
In a situation where the survival rate from cancer has risen owing to advances in medicine, and the expected survival of older patients with cancer is increasing, measures to improve their diagnosis, treatment, survival process, and QoL should be devised. Older patients with cancer have certain characteristics that clearly differ from the coping patterns of younger patients with cancer; as such, medical staff need to recognize these characteristics and provide medical services tailored to older patients with cancer. Furthermore, it is necessary to design customized exercise interventions, diet education programs, and psychological support that can improve the QoL of older patients with cancer.
Notes
Authors' contribution
Conceptualization or/and Methodology - YHH, KJM; Data collection or/and Analysis - YHH, KJM; Writing–original draft or/and review & editing - YHH, KJM
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) founded by the Ministry of Education (grant #2019R1I1A3A01060561).
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
None.