Recovery experience of older adults with COVID-19: A grounded-theory study
Article information
Abstract
Purpose
This study aimed to understand the lives of recovered COVID-19 patients from the viewpoints of people over the age of 60.
Methods
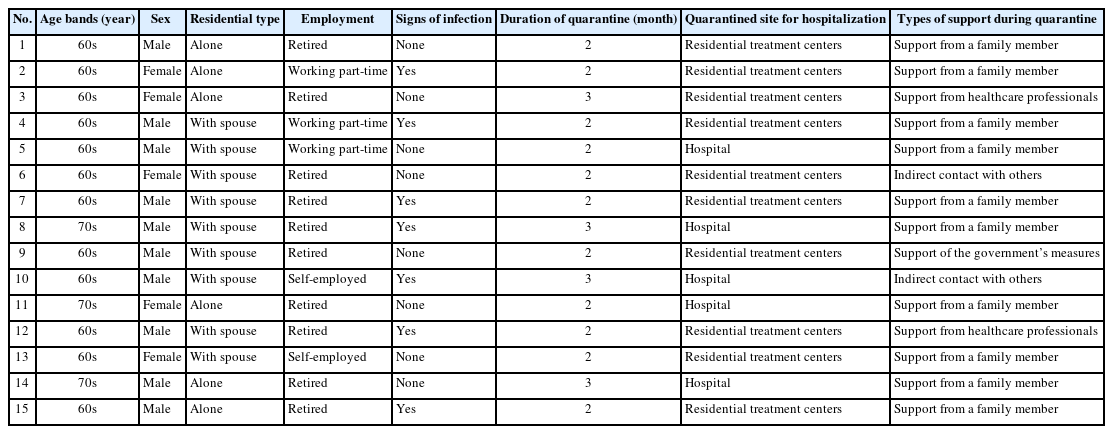
The participants were 15 recovered patients aged over 60 who had been infected with COVID-19. Data were collected individually through in-depth interviews from September 12, 2022 to February 27, 2023. Contents of the transcribed interviews were analyzed using Corbin and Strauss’s grounded theory approach.
Results
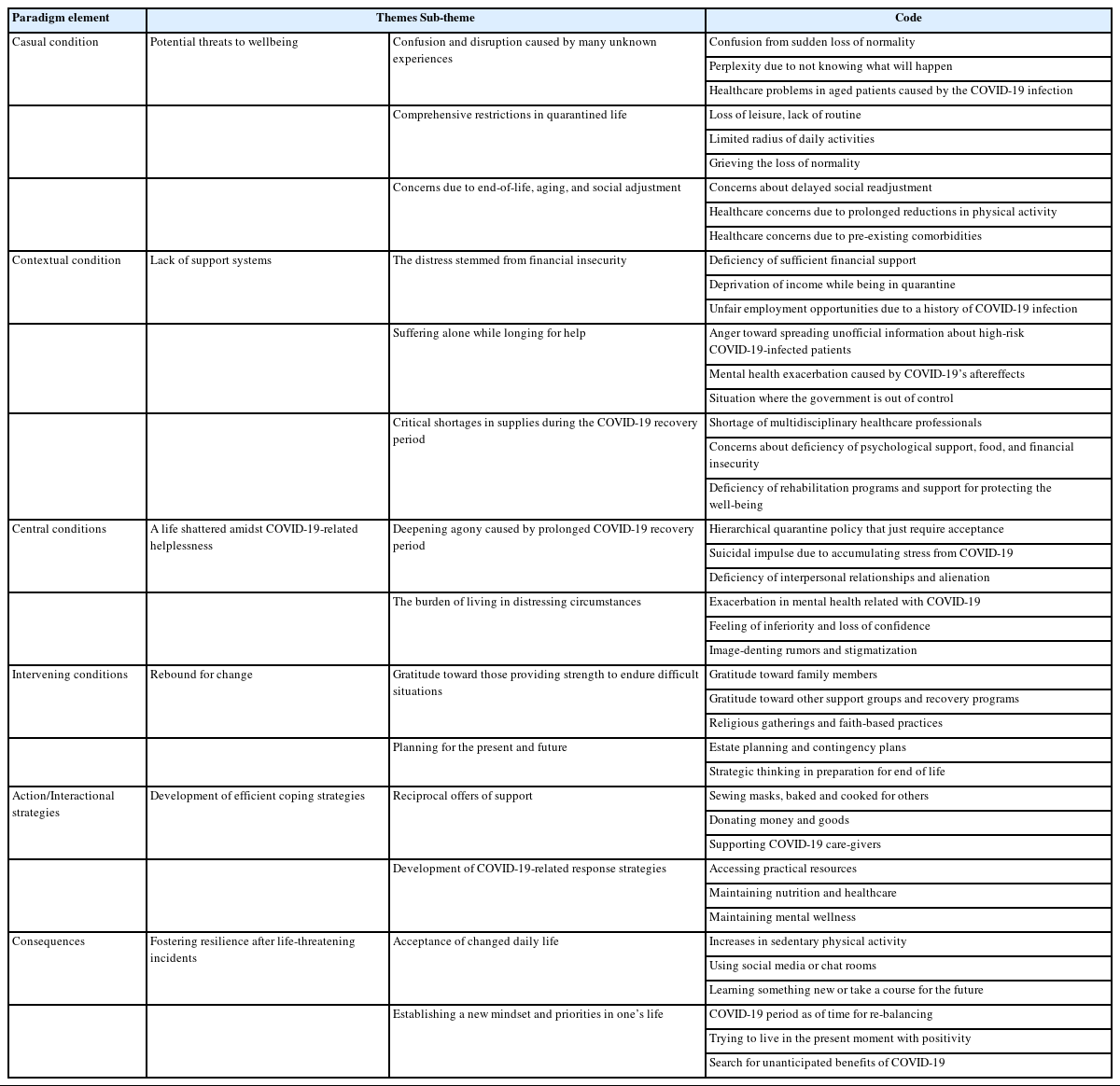
Analysis of the psychological recovery experience for older adults with COVID-19-resulted in six themes, 14 sub-themes, and 41 codes. The core category revealed was turning crisis into opportunities throughout making meaning of living in the time of COVID-19. The causal conditions included feeling disrupted due to unknowns during a crisis. The contextual conditions were a lack of support system for COVID-19 groups. The central phenomenon was a life shattered amidst COVID-19-related helplessness. The intervening conditions were rebound for changes for transformation. As a result, the action/interactional strategies were employed to find a breakthrough. In consequence, enhancement of resilience was achieved after overcoming obstacles.
Conclusion
The findings provide important recommendations for healthcare professionals regarding older patients who have had COVID-19. We encourage healthcare providers to improve patient care by gaining a deeper understanding of their recovery experiences.
INTRODUCTION
Stringent public health strategies to limit COVID-19 transmission have resulted in adverse consequences, particularly for aged patients with COVID-19 and chronic comorbidities, whose voices and perspectives are often unheard [1]. Older patients have higher risks of mortality, comprehensive insecurities after retirement, and exclusion from social and public engagements [2]. A previous study indicates that older patients with COVID-19 are vulnerable to infectious diseases. It shows that aging is closely related to COVID-19 severity, long-term hospitalization, the need for intensive care to support daily requirements, and higher mortality rates [3]. Systematic reviews and meta-analysis results also suggest that aging is related to higher emotional distress [4].
As COVID-19-related long-term hospitalization requires intensive care to support daily requirements, older adults showed adverse outcomes owing to forced hospitalization or quarantine measures. The quarantined situation due to the COVID-19 crisis can influence multiple psychological dimensions in older patients [5]. A previous study indicates that older adults have difficulty adapting to significant life changes after quarantined circumstances [6]: the restricted use of community resources, enforced social isolation, aggravated loneliness, and disrupted outdoor activities, adversely affecting mental and physical health. Researchers have demonstrated that older adults with COVID-19 in forced situations are susceptible to generalized anxiety disorder [7]. In particular, forced hospitalization or quarantine measures cause older adults to be exposed to anxiety disorders, depressive disorders, sleep-wake disorders, and trauma, stressor-related disorders which prolong the impact of COVID-19 [8]. Previous research reported that the recovery of psychological symptoms for older adults in quarantined circumstances are more complicated and maintained in the long-term [9]. Hence, effective ways to understand psychological distress in older adults with a history of COVID-19 who have undergone quarantine, and support their life changes are essential. The voices and perspectives of older adults with COVID-19 during quarantine measures have often been overlooked, and they are likely to experience widespread stressors in managing the COVID-19 crisis. However, given that COVID-19 is a novel disease, limited qualitative studies have been conducted to develop theories to understand the recovery process [10]. Therefore, understanding effective ways to understand their psychological health, emotional well-being, and resilience from forced restriction is essential.
Apart from previous research methods, the qualitative study using a grounded theory approach aims to provide clear guidelines for complex phenomena by linking particular constructs and developing new strategies. It enables a comprehensive understanding of the research phenomenon to develop effective intervention strategies to promote rehabilitation in times of trauma [11,12]. The purpose of this study is to explore how individuals aged 60 and above navigate their coping mechanisms during the COVID-19 crisis within the domestic sociocultural context. We aimed to understand the underlying psychological insights in the context of COVID-19 and promoting an understanding of the recovery process of older patients in critical situations. Therefore, we adopted a grounded theory approach to understand the experiences of older adults with a history of COVID-19 and lay the groundwork for developing nursing intervention programs specifically designed for older adults aged 60 and above affected by COVID-19.
METHODS
Ethic statement:This study was approved by the Institutional Review Board (IRB) of the Kyungpook National University (No. 2022-0320). Informed consent was obtained from the participants.
1. Study Design
The authors complied with consolidated criteria for reporting qualitative research (COREQ) guidelines. This qualitative study employed Corbin and Strauss’s [12] methodology for grounded theory qualitative research, to describe the relationships between concepts that constitute the phenomenon and investigate the recovery process of older adults with a history of COVID-19. Through examining and exploring various perspectives on individuals’ behaviors, researchers can scrutinize these behaviors and develop a comprehensive, situation-specific theory. Through a grounded theoretical approach, the researcher can develop a theory that can explain complex and multi-dimensional situations by exploring the experiences of older adults with a history of COVID-19.
2. Setting and Sample
A total of 15 participants were recruited based on purposive and snowball sampling. The recruitment was conducted in a way that previously recruited participants recommended subsequent participants. A total of 10 participants were recruited based on verbal referrals from participants who had previously been recruited, and the other five participants were subsequently recruited based on the recommendation of G wellness centers’ staff members.
In grounded theory, participant selection is an important procedure achieved through theoretical sampling that deliberately selects appropriate study participants. Theoretical sampling is a process for researchers to determine data to collect based on analyzing prior data to decide the next collection target within a particular context [11]. According to theoretical sampling methods, subsequent data were determined based on the analysis of the characteristics, and quality of previous data. By analyzing samples intentionally collected based on concepts, researchers can discover common core concepts by extracting attributes from study participants [11,12].
Afterward, analyzed data were theoretically saturated based on continuous comparative analysis of information until new meaningful information was no longer yielded. Theoretical saturation occurs when the development of all paradigm categories becomes densely woven, and no new or related data emerges. At this stage, relationships between categories are well-established, and new meaningful information is no longer yielded [12]. We reached theoretical saturation after analyzing data up to the 15th participant, where the data no longer yielded new concepts or themes.
Inclusion criteria included older adults aged 60 and above who had recovered and could truthfully describe their experience of being quarantined due to COVID-19. We included participants who could reflect on their experience and signed the consent form. Based on considering the recovery from traumatic experiences, we recruited participants who have been maintaining their daily lives without problems for at least one year after being quarantined [13,14]. Accordingly, we recruited participants who had been forced to quarantine due to COVID-19 from January 2021 to August 2021. In addition, we conducted a psychological test in advance provided by G wellness center to include participants for those who fall within the normal range [15]. Exclusion criteria included those with cognitive impairment or a diagnosis of post-traumatic stress disorder (PTSD) due to psychiatric stress caused by COVID-19.
3. Ethical Considerations
This study was reviewed and approved by the Ethics Committee of Kyungpook National University (IRB No. 2022-0320). The researchers explained the study’s purpose, methods, and their right to stop participating at any time without disadvantages to the participants. Their willingness was confirmed by obtaining their signatures on informed consent forms. The recorded data were kept in a password-protected file and paper-based documents in a locked cabinet.
4. Data Collection
Data collection was conducted from September 12, 2022 to February 27, 2023, by using face-to-face, individual, semi-structured interviews. As the potential risks of quarantine experiences were weighed carefully against possible distress, we interviewed three older adults with a history of COVID-19 for pilot testing in August. Previous studies have reported that PTSD related to COVID-19 can cause past trauma to suddenly appear. In addition, it causes abnormal symptoms such as suffocation [8]. All interviews were conducted in the counseling room within the hospital affiliated with the G wellness center where medical treatment was available in the event of an emergency to alleviate COVID-19-related risks. Multidisciplinary experts (nursing professors and psychologist) participated in discussions to determine the research participants. First, background information—living situations, patient history, the status of physical and mental health—was assessed to determine the study participants’ availability of interviews.
Next, to build a rapport, researchers were introduced, psychological support guidelines were provided, participants’ written consent was obtained, and interviews were scheduled at their convenience. Interviews (up to three sessions lasting 60 to 90 minutes per person) were conducted complying with COVID-19 safety guidelines by the research member who previously worked in a COVID-19 ward—wearing masks and temperature checks.
The researchers began the interviews by empathically asking open-ended questions and ended them by expressing appreciation for the participants’ engagement. The main interview questions were “What have you been through sequentially after the infection?” and “What are your coping strategies?”, “What was the most difficult part of the COVID-19 infection period?”, and “What change did you feel through the COVID-19 experience?”. The frequently used facilitation question was “Is there anything else you want to talk about regarding COVID-19 experience? If so, “please tell us?” All interviews were audio recorded. The interviewer summarized the content, asked the participants to confirm it, and made debriefing notes after each interview. Psychological guidance materials were sent after the interview to assess participants’ mental states, and if applicable, post-interviews were implemented to reduce potential trauma risks.
5. Data Analysis
To identify and classify similarities and differences in data and extract distinct categories for interpretation, researchers use the constant comparison method.
First, the outline centered on psychological pain among adults with a history of COVID-19 who had been quarantined was formulated after several readings of the interviews, excluding researchers’ prejudices. Transcripts were returned to participants for comment and correction. Data analysis was conducted based on Corbin and Strauss’s qualitative research methodology with a grounded theory approach [12]. Thereafter, interviewers reviewed all the transcripts using the QSR NVivo11 program for open coding [16]. In data analysis, codification procedures, such as simple word-by-word and line-by-line coding, were also implemented.
Open coding is an analytical approach that involves naming and categorizing phenomena during the initial phase of coding through close data examination. This process involved carefully reviewing and re-reviewing the raw data multiple times. Open coding enables in-depth analysis by deriving categories through event-to-event and object-to-object comparisons, along with the use of theoretical comparison techniques. Similar or different concepts were compared to derive a particular category, find and classify differences in their attributes using theoretical comparison techniques. This allowed us to group similar concepts, forming broader categories. Through open coding, specific concepts (codes, sub-themes, themes) emerged from the raw data, revealing their properties and dimensions.
In axial coding, the process involved reassembling previously distinct concepts and categories that had been derived through open coding to construct a structural framework. This framework was developed to provide a more detailed and comprehensive explanation of the phenomenon under study. Axial coding involves connecting categories through a paradigm model, including crucial elements such as causal conditions and consequences.
A causal condition refers to an event that triggers or facilitates a particular phenomenon. Contextual conditions refer to the set of circumstances or environments in which a particular phenomenon is situated. Intervening conditions within a specific context can either facilitate or inhibit the effectiveness of action/interaction strategies. Action/interaction strategies involve addressing, controlling, executing, and responding to a phenomenon. Consequences refer to the results that stem from the action/interaction strategies.
In the selective coding phase, the content at the descriptive level was developed to an abstract level. We identified a core category that represents concepts and categories. All categories were integrated around the core category using selective coding. We used this core category as the foundation to create a theory, focusing on the recovery process of older adults with COVID-19 in our study.
Afterward, process analysis was conducted to understand how participants’ experiences evolved over time. A process analysis involves linking stages sequentially over time. This approach enables us to comprehend how the process evolves under the influence of variables to lead to an outcome.
6. Rigor
To enhance rigor, Guba and Lincoln’s [17] criteria of truth value, applicability, consistency, and neutrality were used. Truth value was confirmed through repeated checks and interpretations for accuracy. The interview transcripts were analyzed, and their accuracy was strengthened by obtaining the participants’ reaffirmation. Applicability of the results was established by obtaining confirmations from three participants and three non-participants to enhance authenticity so that the results could be applied to a wider range of situations. Consistency was determined by theoretical comparisons. Throughout the analysis, the data and coding were regularly checked by researchers, nursing professors, and a psychologist. Neutrality was maintained by avoiding involvement/interactions between the researchers and participants. To exclude prejudices, all reflections were recorded, and the research process was noted, which helped to avoid biases.
RESULTS
The 15 participants were 60 years and older (Table 1). Six themes, 14 sub-themes, and 41 codes (Table 2) were identified.
1. Casual Condition: Potential Threats to Wellbeing
Older patients who were infected with COVID-19 faced a growing sense of anxiety about their physical and mental well-being due to the effects of confinement. Those who were isolated in hospitals witnessed COVID-19-related deaths, which made them more aware of the severity of the infection. They expressed a sense of emotional despair because they had nowhere to turn for straightforward guidance on what to do next, and they lacked outlets for emotional support. Amidst the confusion during confinement, participants were worried about the prospect of returning to society and resuming their usual lives.
1) Confusion and Disruption Caused by Many Unknown Experiences
Many participants longed for the normalcy of their pre-COVID-19 lives. Others described concerns about additional age-related COVID-19 risks. They requested support plans for older patients including psychological interventions to alleviate mental stress. Although they were confused by the disruption of their daily lives due to COVID-19 infection, they revealed that they lacked information and guidance from healthcare professionals.
Although I needed help and attempted to reach out to the relevant department, I found it challenging and lacked sufficient information on the necessary steps to take. It would be beneficial if information could be disseminated effectively, aiding older adults in coping with COVID-19. (Participant 1)
COVID-19 disrupted our daily routines and it was really hard to try and get it all set up. (Participant 2)
2) Comprehensive Restrictions in Quarantined Life
Considering their vulnerability to infectious diseases and compliance with social distancing guidelines, participants had experienced a loss of their usual routines at restricted places. Participants experienced significant challenges and setbacks in adapting their daily routines to a new normal with many fearing reductions in their radius of daily activity.
I was completely isolated. There was a huge pile of COVID-19 patient files on the COVID-19 ward, and all the medical staff was wearing protective clothing. (Participant 7)
I feared the extent of unwanted governmental privacy regulations. (Participant 11)
3) Concerns Due to End-of-Life, Aging, and Social Adjustment
In combination with pre-existing comorbidities, the majority of participants feared health risks, viewing aging and frailty as closely linked to an increased mortality rate from COVID-19.
I realized that I’m old. What I’m afraid of is that with age, I may need intubation. (Participant 1)
As I have lifelong complications, I am often put on ventilators, and a feeding tube during hospitalization. The longer this repetition lasted, the more despair overcame me. (Participant 5)
I’m worried about whether I can adapt like before COVID-19 because I’ve lost contact with people and I haven’t had any social exchanges for months. (Participant 13)
2. Contextual Condition: Lack of Support Systems
Many people found themselves spending time in self-isolation, using COVID-19 self-test kits to determine if they were positive or negative. The limitations on social interactions during isolation also resulted in unavoidable financial losses. When trying to access economic assistance, they mentioned that the government’s eligibility criteria were complicated, making it challenging to qualify. Moreover, government guidelines have undergone frequent changes, and officials in charge have often been unreachable by phone. It was common that temporary support was sometimes offered but then abruptly disappeared. Older patients, in particular, required more support than younger individuals, yet aside from isolation, they received minimal assistance.
1) The Distress Stemmed From Financial Insecurity
Most participants expressed significant emotional distress due to not receiving adequate living allowances. The financial assistance provided to offset the impact of the COVID-19 quarantine was insufficient to cover the size of the loss incurred during the quarantine period.
Due to old age and the stigma associated with being infected with COVID-19, participants also experienced difficulties in returning to their previous jobs and faced rejection while searching for new employment. Participants experienced insufficient income while under quarantine and struggled with the burden of sustaining their livelihoods.
I did not receive any financial support during my quarantine due to COVID-19. I’ve been quarantined for a long time, I’m concerned about not having enough funds for use once I’m released. (Participant 8)
I’m looking for a new job, but my previous company rejected me due to my history of COVID-19 infection. Moreover, the rumor that I was infected with COVID-19 and quarantined seems to have a negative impact on my job search. (Participant 11)
2) Suffering Alone While Longing for Help
The participants found that they were socially stigmatized for being infected with COVID-19 and were psychologically wounded by constant stories about groups with COVID-19, even after their release from quarantine. Participants felt that, in reality, it is difficult to receive tangible help, and they ultimately believed they had to manage everything on their own.
People do not approach me because of the prejudice that it is transmitted more quickly from older adults infected with COVID-19. (Participant 8)
I had hoped the number of places where I could consult would increase while restricted. (Participant 15)
3) Critical Shortages in Supplies During the COVID-19 Recovery Period
Inadequate support from healthcare professionals and rehabilitative programs, and the lack of essential supplies worsened the predicament causing significant physical and emotional stress for older patients. Participants often mentioned experiencing sudden emotional changes, such as anxiety and depression. They believed that having more outlets for receiving kind words and emotional support would help them find emotional stability.
I didn’t get enough necessities and financial support needed for my daily life. It took a long time to receive them. There was no emotional connection either. (Participant 8)
When I felt helpless, I hoped I could talk with healthcare workers or use rehabilitation services. The harder the situation was, the more desperately I needed someone to rely on. (Participant 2)
3. Central Phenomenon: A Life Shattered Amidst COVID-19-Related Helplessness
Participants expressed stress during their COVID-19 recovery period, which lasted for more than a month. The majority of participants reported that they had to comply with a hierarchical quarantine policy that just required acceptance within a confined environment, limiting freedom of expression. Some participants mentioned experiencing extreme stress and suicidal impulses because of the adverse situation they experienced due to COVID-19. Participants reported experiencing personality changes in a negative direction. They also faced a lack of interpersonal relationships, along with damaging rumors and stigmatization related to COVID-19. The social stigma associated with contracting COVID-19 led to feelings of insignificance and a loss of confidence, contributing to participants’ sense of alienation from acquaintances after their release from quarantine.
1) Deepening Agony Caused by Prolonged COVID-19 Recovery Period
The government imposed residential restrictions and enforced isolation from acquaintances during the recovery period, all justified by the need to prevent further virus spread. Most of the participants confessed that it was hard to recall their experiences in quarantine facilities which they were unable to escape from. This situation, coupled with uncertainty about their futures, led to elevated levels of depression and diminished self-esteem. In some cases, participants even contemplated extreme actions like suicide, feeling as if they were pushed to the edge of their lives
Tears began to flow as I found myself compelled to take unwanted medication and undergo periodic blood pressure checks by the medical staff in the isolation room consistently. (Participant 8)
I often experienced nightmares, and negative thoughts plagued my mind, leading to overwhelming despair. Sometimes, I felt the desire to die whenever the painful memories emerged. (Participant 10)
After the COVID-19 infection, the shift to a completely non-face lifestyle led to feelings of isolation and emptiness, with limited opportunities for in-person social interaction. There were days when everything felt monotonous, and I lacked someone to have a conversation with. (Participant 11)
2) The Burden of Living in Distressing Circumstances
They expressed their distress about being confined to limited spaces with very limited engagement they could do due to the sudden changes in their daily lives. They experienced a sense of insignificance and a loss of confidence. The confined situation combined with image-denting rumors and stigmatization evoked severe fear, leaving their mental well-being in a fragile state.
I was mentally exhausted, discouraged, and had lost confidence in living due to the prolonged distressing situation associated with COVID-19. It felt like I was insignificant. (Participant 5).
People avoid approaching me due to the prejudice that COVID-19 is particularly contagious among older adults with a history of the virus. Consequently, I felt alienated by acquaintances around me. (Participant 8)
4. Intervening Condition: Rebound for Change
Support and encouragement from religion and family have been instrumental in their lives, serving as strong pillars and sources of motivation. They’ve also come to rely on external support, which has strengthened their belief that they can overcome challenges. Due to their old age, some participants made financial arrangements to prepare for the potential worsening of their health. They also devised temporary solutions in anticipation of health decline. They focused on healing their minds and souls while taking care of their physical and mental well-being as part of their journey to recover from the consequences of the COVID-19 infection.
1) Gratitude Toward Those Providing Strength to Endure Difficult Situations
They ascribed regaining their vitality to the efforts of support groups, rehabilitation programs and found solace through family. In the participants’ lives, the encouragement from friends and the support of their families served as reliable pillars and sources of motivation. Participants faced challenging emotions like anxiety, fear, insomnia, increased suspicion, reduced engagement in external activities, and feelings of helplessness due to COVID-19. To cope with these difficult emotions, they sought to confide in and communicate with trusted family members, friends, and people in their surroundings.
I’m thankful to my wife who selflessly assisted me by taking care of even the smallest things, enabling me to concentrate solely on my recovery. (Participant 6)
I attend counseling programs via Zoom and find it extremely helpful to share with others. Social media and chat rooms were ways to connect with community members. (Participant 12)
2) Planning for the Present and Future
Participants’ coping strategies in response to the crisis are based on years of accumulated experiences and contingency plans according to the present situation. They were determined not to forget the lessons learned from their past experiences and to strive for a better life than they have now. Simultaneously, few were prepared for the future by making provisions for their families, such as inheritance planning in case of unexpected circumstances.
Coping strategies included making plans for sickness and sharing wishes. I want my family to know my wishes and inheritance documents related to the end of my life. (Participant 9)
To protect my wife, I set up a contingency plan in case I die from COVID-19 by reviewing and writing estate plans, wills, and medical care directives. (Participant 6)
5. Action/Interaction Strategies: Development of Efficient Coping Strategies
Through the experiences they’ve had in life, the participants have fluently developed effective strategies for dealing with difficult situations. They found a sense of purpose and belonging through volunteer activities and charitable contributions after being infected with COVID-19 to overcome feelings of helplessness. Additionally, during the quarantine period, they engaged in indoor exercises, sought online counseling to relieve anxiety and loneliness, and explored various activities like internet searches, and music via their smartphones. Some even reached out to mental health professionals through online. Joining online forums to ask health-related questions and seek answers became a common practice.
1) Reciprocal Offers of Support
Participants’ coping strategies included using the COVID-19 support platforms to feel purposeful and help others. Regular volunteer activities proved to help relieve the stress experienced by participants. The relationships formed through volunteer work sometimes lasted for more than a year and also served as a window for information exchange with the world. Despite their physical ailments, participants felt a sense of mind control, knowing that they could contribute to society, which made them feel like they were free of under COVID-19-infected situation.
I’ve just been trying to keep busy by donating goods to the neighborhood. I’m restricted due to COVID-19, but fulfilled by donating to others. (Participant 14)
I’ve contacted elected officials by volunteering on political campaigns by posting on social media to offer support and reassurance in expanding support for COVID-19 caregivers. (Participant 11)
2) Development of COVID-19-related Response Strategies
Physical and mental health were important priorities. Some participants approached mental wellness centers in times of difficulty. Conducting activities was described as an effective coping strategy. Participants took online courses, learned how to use multimedia devices, and diverted their attention from the disease through hobbies. Researchers and community healthcare providers have provided the acquisition of coping skills to older patients, continue improving their awareness, and investigate their responses during recovery.
After being diagnosed with COVID-19, I reached out to crisis helplines and community psychiatric support for assistance with depression and recovery from the extended illness. (Participant 10)
Focusing on the activities helped me. Getting projects started and completed has been instrumental in the rehabilitation period. (Participant 6)
6. Consequences: Fostering Resilience After Life-Threatening Incidents
The COVID-19 crisis experience has brought about a shift in thinking, allowing individuals to discover positive aspects even within the crisis itself. They also experienced the satisfaction of persevering and achieving something even in the face of adversity.
1) Acceptance of Changed Daily Life
Participants faced challenges of finding “equivalent” activities to maintain their physical activity routines. Time spent in sedentary activities increased after COVID-19’s onset. The wisdom and insight of older adults, accrued from various life experiences, acted as an important positive factor in their adaptation. Most participants gradually sought their own leisure and peace of mind as they embraced the inevitable reality in their daily lives. They appeared to experience the major life-threatening event more positively and willingly adjusted to their situation.
I discovered a new way to do yoga without spending money on gym. I’m spending much time on joining online yoga classes. (Participant 3)
I was looking at alternatives to keep active. Home improvement projects have been instrumental in my sanity. This keeps my mind busy and off of trace of COVID-19. (Participant 12)
2) Establishing a New Mindset and Priorities in One’s Life
Changing one’s perspective of the COVID-19 crisis and regarding it as an opportunity to overcome adversity were important factors in the adaptation process.
I think… there are some little positive benefits. I’m not rushing around so much anymore, it’s given me the time and the opportunity to notice small things. (Participant 9)
I cherish this moment and try to live faithfully in the present. I learned to live with considerable challenges with patience while dealing with crises. “Every cloud has a silver lining.” (Participant 7)
7. Process Analysis
The core category revealed was turning crisis into opportunities throughout making meaning of living in the time of COVID-19. Although time cannot heal all wounds, it allows participants to experience events, form new perspectives, and reorient for the future. Participants reflected on their lives and became stronger by enduring various aspects of pain related to COVID-19. Acknowledging the unavoidable and reorienting to changes were identified as the core categories, with the strategic coping process comprising three stages: recognition of crisis, seeking a way out, and fostering resilience (Figure 1).

Turning crisis into opportunities throughout making meaning of living in the time of COVID-19 pandemic.
1) Recognition of Crisis
Participants said they felt fear as a representative after-effect of COVID-19. The unprecedented global epidemic has been life-threatening because there is no treatment other than vaccination. The stigmatization of groups for COVID-19 infection has intimidated participants. Participants confessed that they did not know how to cope with the aftereffects of COVID-19 infection and protect themselves. Moreover, they experienced pain caused by the various inevitable changes in their lives and the guilt that negatively affected their families.
2) Seeking a Way Out
Some participants acknowledged it was important to comply with COVID-19 regulations, even though these regulations were unbearable in daily life. Assuming a relaxed attitude toward the disease, ensuring they received appropriate rest, and volunteering were activities that reinvigorated participants, and helped them establish a daily routine.
3) Fostering Resilience
Participants occasionally experienced feelings of unease as a consequence of using various coping strategies. However, with time, they gained resilience while dealing with the emotional turmoil caused by the COVID-19 infection, and accepted the inevitable changes. Participants found peace of mind and increased their quality of life by designing a long-term plan and not dwelling on the current crisis.
DISCUSSION
This study utilized Corbin and Strauss’s grounded theory approach to explore the recovery process of older patients who have experienced forced quarantine.
In the casual condition, potential threats to wellbeing during COVID-19 emerged as upper themes. Studies found negative psycho-social health consequences, including anxiety, depressive symptoms, social isolation, and loneliness due to the disease’s unprecedented circumstances [18,19]. Congruent with international research, most of this study’s participants reported confusion from the sudden loss of normality, not knowing what would happen, and healthcare problems during COVID-19 recovery [20]. This suggests that adequate guidelines must be provided to alleviate confusion by the aftereffects of COVID-19. Some participants were concerned about their COVID-19 infection and its complications affecting their pre-existing health conditions, and leading to death. Healthcare professionals should consider unique characteristics like aging and frailty of older adults with COVID-19, and provide adequate support.
In the contextual condition, lack of support systems for older patients emerged as upper themes. We found that participants experienced distress that stemmed from financial insecurity and suffering alone while longing for help during the COVID-19 recovery period. Older adults with a history of COVID-19 suffered alone due to long-term quarantine, mental health exacerbation, challenges in accessing adequate information to cope with crises, and a deficiency of vital supplies that were out of stock. The deprivation of income, reduced social opportunities, and unfair employment opportunities due to a history of COVID-19 infection were frequently shown to adversely affect the rehabilitation and integration into society for adults with a history of COVID-19 [21]. This situation made it especially challenging for older patients, as they had to navigate through the ongoing and unpredictable nature of the COVID-19 crisis with limited resources. In this regard, a phone line or online service, managed by healthcare providers and subsidies specifically designated for older adults recovering from COVID-19, could offer information to reassure patients, thereby facilitating their reintegration into society. Moreover, this suggests that healthcare professionals must provide a continuous provision of medical supplies and standardized guidelines to ensure that older patients respond appropriately to the changed environment.
In the central phenomenon, a life shattered amidst COVID-19-related helplessness emerged as an upper theme. Participants were psychologically burdened by negative social biases and struggled to accept that they were infected with COVID-19. In this regard, previous studies have mentioned widespread discrimination against older adults with a history of COVID-19 [22]. This emphasizes the need to educate the general public to prevent the spread of misinformation and misconceptions about COVID-19. Individuals who were alienated or quarantined in the COVID-19 recovery period often experience chronic mental illness while recovering from this life-threatening experience [23]. This implies the significance for public healthcare professionals to adopt a therapeutic communication approach, as psychological support has the potential to gradually alleviate feelings, such as fear, worry, and suicidal thoughts. The unspecialized, top-down, and authoritative guidelines also implied a need for a stronger social safety net. Therefore, it is crucial to establish structural measures for the continuous monitoring of older patients who have faced the COVID-19 crisis, and structural efforts are needed to assist them during their COVID-19 recovery period.
In the intervening condition, reframing one’s value for life, and encouraging specific strategies to cope with adversities emerged as upper themes. A previous study stated that family and social support served as psychological pillars in overcoming the COVID-19 crisis [24]. A previous study found that most older adults with a history of COVID-19 believed that an appropriate social support system played an important role in coping with crises [25]. This study found that the participants’ accumulated experience and life wisdom served as a buffer, allowing them to accurately recognize the current difficulties and overcome uncertain situations [26]. Therefore, health professionals must focus on older adults with a history of COVID-19, employing secondary strategies to adjust their outlook on planning for different scenarios to accommodate future uncertainties.
For coping, life adjustment, and rehabilitation, participants voluntarily developed action-interactional strategies. A previous study indicated that most older adults with a history of COVID-19 tried to overcome the crisis by focusing on something socially contributable, which played a decisive role in responding to the crisis [26,27]. This study also found interpersonal contact, such as receiving and providing social support, to be a factor influencing stress reduction in older adults with a history of COVID-19. These findings imply that well-established reciprocal support systems play a central role in this population to flexibly adapt to the new environment.
As a consequence of utilizing action-interactional techniques, participants gradually fostered resilience. Moreover, studies have shown that older adults with a history of COVID-19 tried to reevaluate their life priorities and gradually readjusted and accomplished achievable goals while coping with challenges [28]. Most participants regained stability and calmness while controlling the situation in using the latest online devices or encouraged them to find indoor alternatives to their usual outdoor physical activities [29]. Accepting changed situations and maintaining positive self-esteem play a crucial role in fostering resilience [30]. These results show that each patient’s personalized psychological experience should be monitored by healthcare professionals to support them aptly for recovery in response to changed situations.
This study’s strength is that it described unique contexts of the experiences of older adults with a history of COVID-19. This study also has limitations. In this qualitative study focused on an in-depth exploration of the experiences of a small sample. As data could not be collected from a broader geographical area owing to COVID-19 restrictions, the results may not be applied to other patients. Therefore, the findings must be interpreted cautiously to trace further effects among older patients with COVID-19.
CONCLUSION
This study provides a comprehensive and in-depth understanding of the recovery of older COVID-19 patients who were quarantined. It’s evident that these individuals grapple with physical, emotional, and social challenges, all while adapting to changes in their daily lives. We observed that although negative emotions were prevalent at the outset, the deployment of coping mechanisms and psychological maturation played vital roles in the growth to maintain their mental well-being after their quarantine period. Findings offer valuable recommendations for health experts for older patients with COVID-19. We encourage healthcare professionals to provide better healthcare by understanding the experience of their psychological recovery process.
Notes
Authors' contribution
Study conception and design acquisition - HSK; Data collection – HSK and JWP; Analysis and interpretation of the data - HSK and JWP; Drafting and critical revision of the manuscript - HSK and JWP
Conflict of interest
No existing or potential conflict of interest relevant to this article was reported.
Funding
None.
Data availability
Please contact the corresponding author for data availability.
Acknowledgements
We thank interdisciplinary healthcare professionals for analysis and interpretation of the data and supervising the manuscript. We also thank all study participants.